Opening your blood test results and seeing a value flagged as “HIGH” can be an unsettling experience. When that flagged value is your white blood cell count, it’s natural for your mind to race with questions. What does this number mean? Is it a sign of something serious?
Table of Contents
This comprehensive guide from the experts at BloodTestCenter.com is here to demystify your Complete Blood Count (CBC) results. We’ll break down leukocytosis (the medical term for a high WBC count) and explain what it means for your health. While a high white blood cell count is a critical signal from your immune system, its meaning can range from a harmless, temporary stress response to a sign of a significant underlying illness. Understanding the numbers, the different types of white blood cells, and the appropriate next steps is the key to taking control of your health narrative.
Understanding the Basics: White Blood Cells and the Normal Range
Before we can understand what a high count means, we need to understand the basics. This foundational knowledge will empower you to have a more informed conversation with your healthcare provider.
What Are White Blood Cells (Leukocytes)?
Think of white blood cells (WBCs), or leukocytes, as the dedicated soldiers of your immune system. They are the first responders on the scene of any health threat. Produced in your bone marrow, these powerful cells circulate throughout your bloodstream and tissues, constantly on patrol for foreign invaders like bacteria, viruses, fungi, and parasites. Their primary mission is to identify, attack, and destroy these threats, protecting you from infection and illness.
Defining the Normal WBC Range
On your blood test report, your WBC count is measured in cells per microliter of blood (cells/mcL). While the exact numbers can vary slightly from one lab to another (e.g., Labcorp vs. Quest Diagnostics), the generally accepted normal WBC range for adults is:
4,500 to 11,000 cells/mcL
Any value within this range is typically considered normal.
What is Considered a High WBC Count (Leukocytosis)?
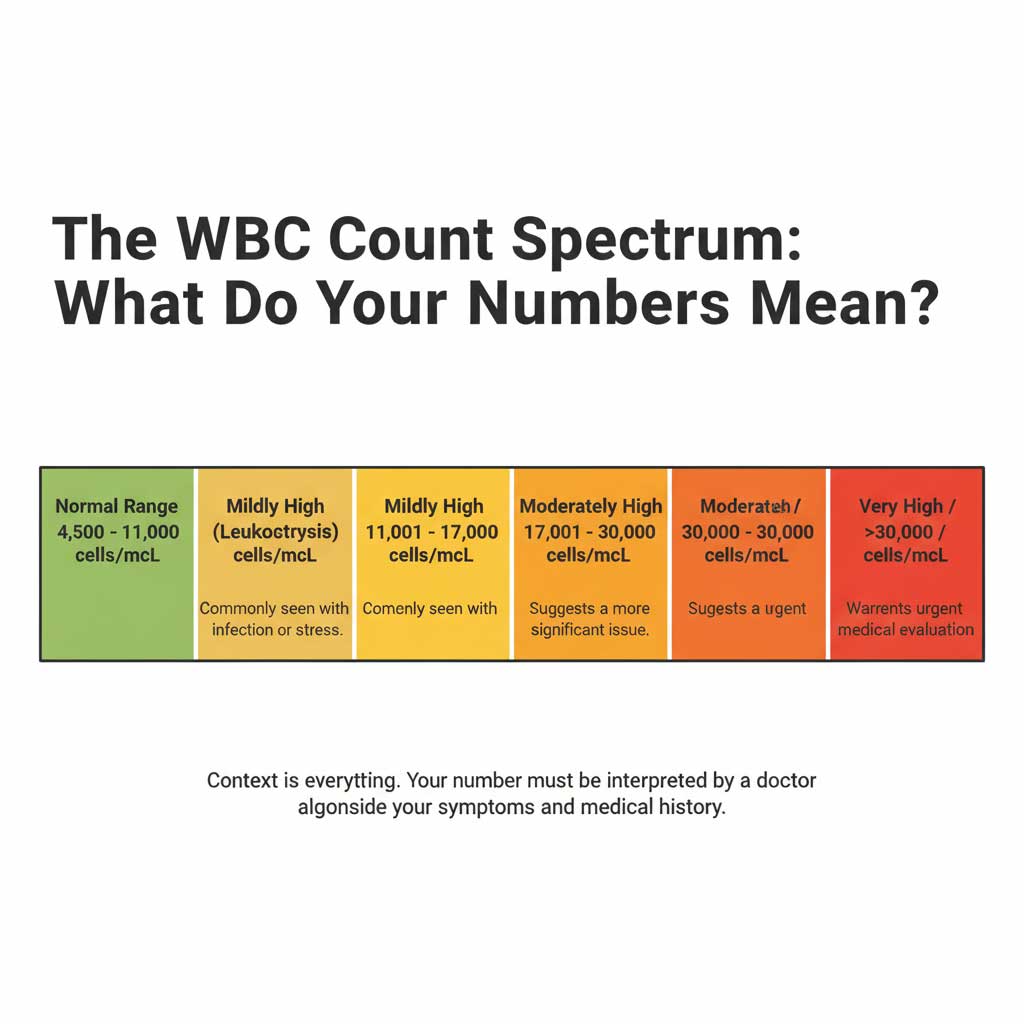
The medical term for a high white blood cell count is leukocytosis. It is clinically defined as any WBC count over 11,000 cells/mcL. However, the degree of elevation is critically important for determining the likely cause. Doctors often think about leukocytosis in tiers:
- Mild Leukocytosis: A WBC count 12000 to 17,000 cells/mcL. This is a very common finding and is frequently caused by a routine infection, significant stress, or inflammation.
- Moderate Leukocytosis: A WBC count between 17,000 and 30,000 cells/mcL. This level suggests a more significant infection or a more pronounced inflammatory response.
- Severe Leukocytosis: A WBC count over 30,000 cells/mcL. This raises more concern and prompts a more thorough investigation for serious conditions.
- Hyperleukocytosis: An extremely high WBC count, typically over 100,000 cells/mcL. This is a critical value and is most strongly associated with blood cancers like leukemia.
Common Causes of a High White Blood Cell Count
A vast majority of cases of leukocytosis are caused by your body’s normal, healthy response to a challenge. Understanding the common leukocytosis causes can help put your results into context.
Infections: The Number One Culprit
By far, the most frequent reason for a high white blood cell count is an active infection. When your body detects a bacterial or viral invader, it sends a signal to your bone marrow to ramp up the production and release of WBCs to fight it off.
- Bacterial Infections: Conditions like pneumonia, urinary tract infections (UTIs), strep throat, or an infected wound are classic triggers for a high WBC count.
- Viral Infections: Viruses like influenza, mononucleosis (“mono”), or COVID-19 also stimulate a strong immune response, leading to leukocytosis.
Inflammation
Inflammation is the body’s natural response to injury or chronic irritation. This process involves a surge of white blood cells to the affected area to clean up damage and begin the healing process.
- Injuries: Significant trauma, burns, or post-surgical recovery will cause a temporary spike in your WBC count.
- Autoimmune Diseases: Conditions where the immune system mistakenly attacks the body’s own tissues, such as rheumatoid arthritis or inflammatory bowel disease (IBD), can cause chronic inflammation and a persistently elevated WBC count.
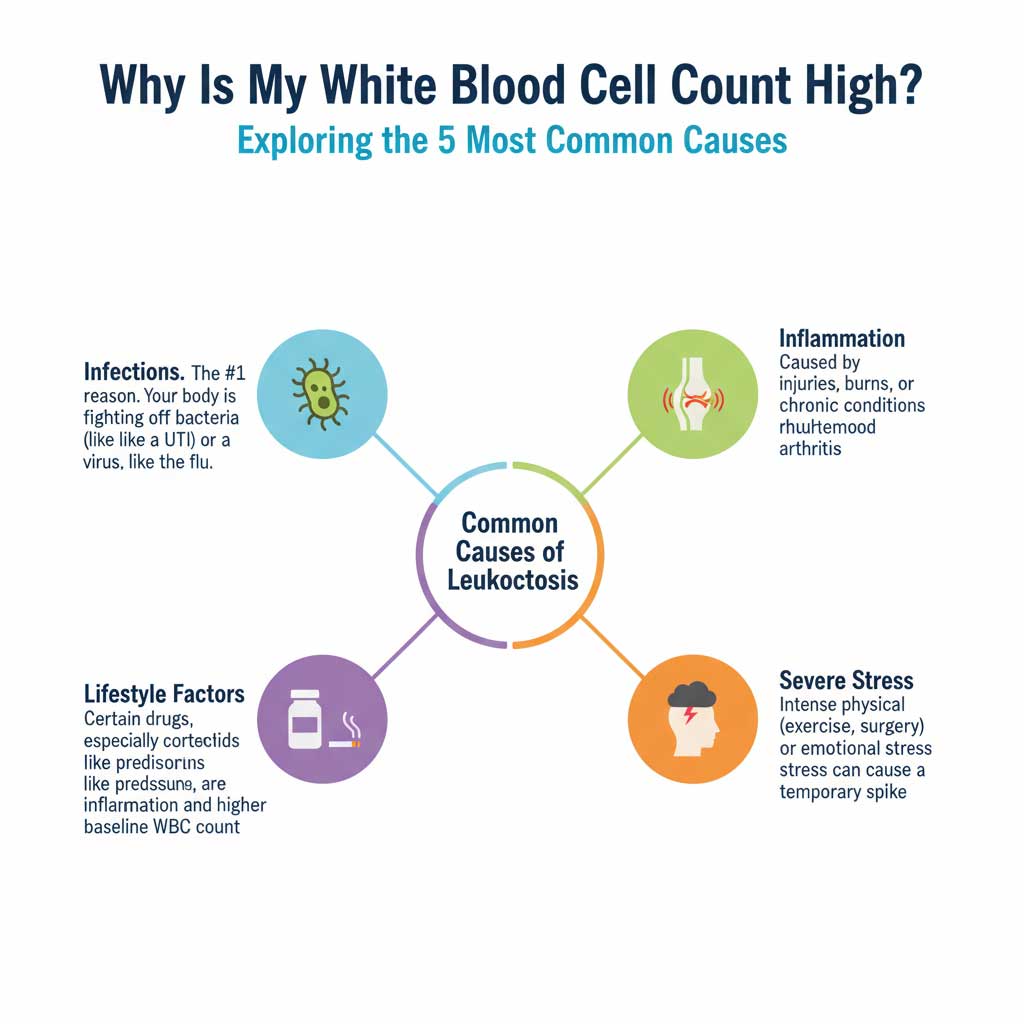
Physical and Emotional Stress
Many people are surprised to learn that stress alone can raise their white blood cell count. When you experience significant stress—whether physical or emotional—your body releases hormones like cortisol and adrenaline. These hormones can trigger the bone marrow to release a stored supply of WBCs into the bloodstream.
- Physical Stress: Intense exercise, surgery, or even a severe lack of sleep.
- Emotional Stress: A common question is, can stress cause high WBC count? The answer is yes. A period of intense anxiety, a panic attack, or severe emotional distress can cause a real, measurable—though typically temporary—increase.
Medications That Increase WBC Count
Several common prescription drugs are known to cause leukocytosis as a side effect. It’s crucial to tell your doctor about every medication you are taking.
- Corticosteroids: Drugs like prednisone are one of the most well-known medications that increase WBC count. They cause the bone marrow to release neutrophils into the blood.
- Other Medications: Lithium (used for bipolar disorder), certain asthma inhalers (beta-agonists), and specialized drugs called colony-stimulating factors (used in cancer patients) also increase the WBC count.
Lifestyle and Environmental Factors
Certain chronic lifestyle habits can lead to a state of low-grade, systemic inflammation, which can result in a baseline WBC count that is higher than normal.
- Smoking: This is a major cause of chronic inflammation throughout the body and is strongly associated with a persistently high white blood cell count.
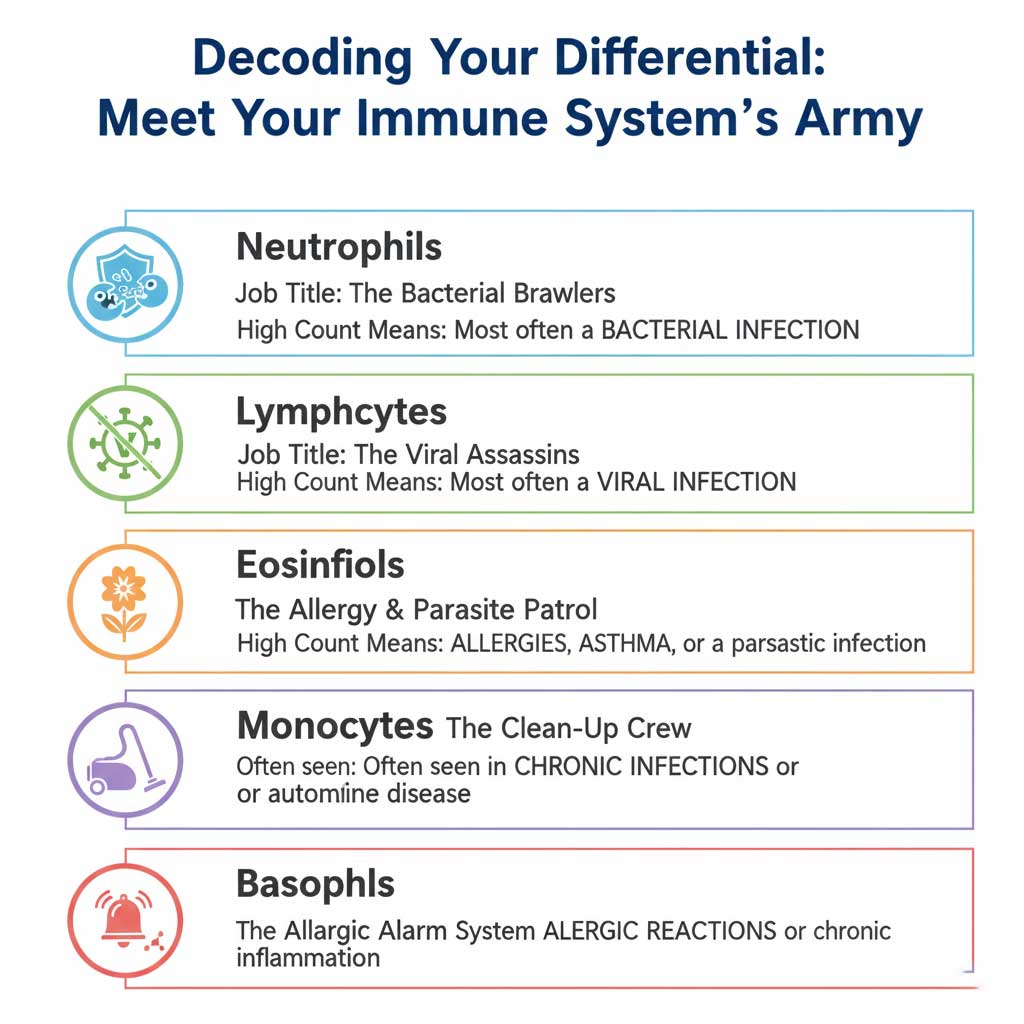
The WBC Differential: The Key to a More Specific Diagnosis
The total WBC count is just the headline. The real story is in the details. A CBC with differential is a crucial test that breaks down your total white blood cell count into its five distinct subtypes. The specific cell type that is elevated provides powerful clues that help your doctor narrow down the potential cause of the leukocytosis. You can easily order this essential test through BloodTestCenter.com to get a complete picture of your immune response.
| White Blood Cell Type | Normal % Range (Adult) | Primary Function | What a High Count (Leukocytosis Subtype) Primarily Indicates |
| Neutrophils | 40% – 60% | Phagocytosis; the “first responders” to infection, engulfing and destroying bacteria. | Neutrophilia: The most common cause of a high WBC count. Classic sign of bacterial infections (e.g., pneumonia, UTI, abscess). Also caused by physical stress, inflammation, steroid use, and smoking. |
| Lymphocytes | 20% – 40% | B-cells produce antibodies; T-cells kill infected cells and regulate the immune response. | Lymphocytosis: Most commonly indicates viral infections (e.g., mononucleosis, influenza, CMV, whooping cough). Can also be a sign of chronic inflammation or specific blood cancers like Chronic Lymphocytic Leukemia (CLL). |
| Monocytes | 2% – 8% | “Garbage trucks” of the immune system; clean up dead cells. Differentiate into macrophages in tissues. | Monocytosis: Often seen in chronic infections (e.g., tuberculosis), autoimmune diseases (e.g., lupus), and certain types of leukemia, particularly Chronic Myelomonocytic Leukemia (CMLL). |
| Eosinophils | 1% – 4% | Fight parasitic infections and are heavily involved in allergic and asthmatic responses. | Eosinophilia: A hallmark of allergic reactions (e.g., hay fever), asthma, eczema, and parasitic infections. Also seen in certain autoimmune diseases and some cancers. |
| Basophils | 0.5% – 1% | Release histamine during allergic reactions and heparin to prevent blood clotting. | Basophilia: The least common type. A high count can be associated with allergic reactions, chronic inflammation (like ulcerative colitis), and is a significant marker for certain types of leukemia, like Chronic Myeloid Leukemia (CML). |
Interpreting Your Differential Results
- What high neutrophils mean: If your report shows neutrophilia, your doctor will first suspect a bacterial infection. This is the classic immune response to bacteria.
- What a high lymphocyte count means: If your report shows lymphocytosis, a viral infection is the most likely culprit.
- What a high eosinophil count means: If your eosinophils are elevated, your doctor will likely ask about allergies, asthma, or recent travel (due to the risk of parasites).
When a High WBC Count is a Red Flag: Leukemia and Other Serious Conditions
It is completely normal for your first thought to be about cancer. While it’s important to be aware of this possibility, it is crucial to remember that the vast majority of cases of leukocytosis are not caused by cancer. Here’s how doctors begin to differentiate.
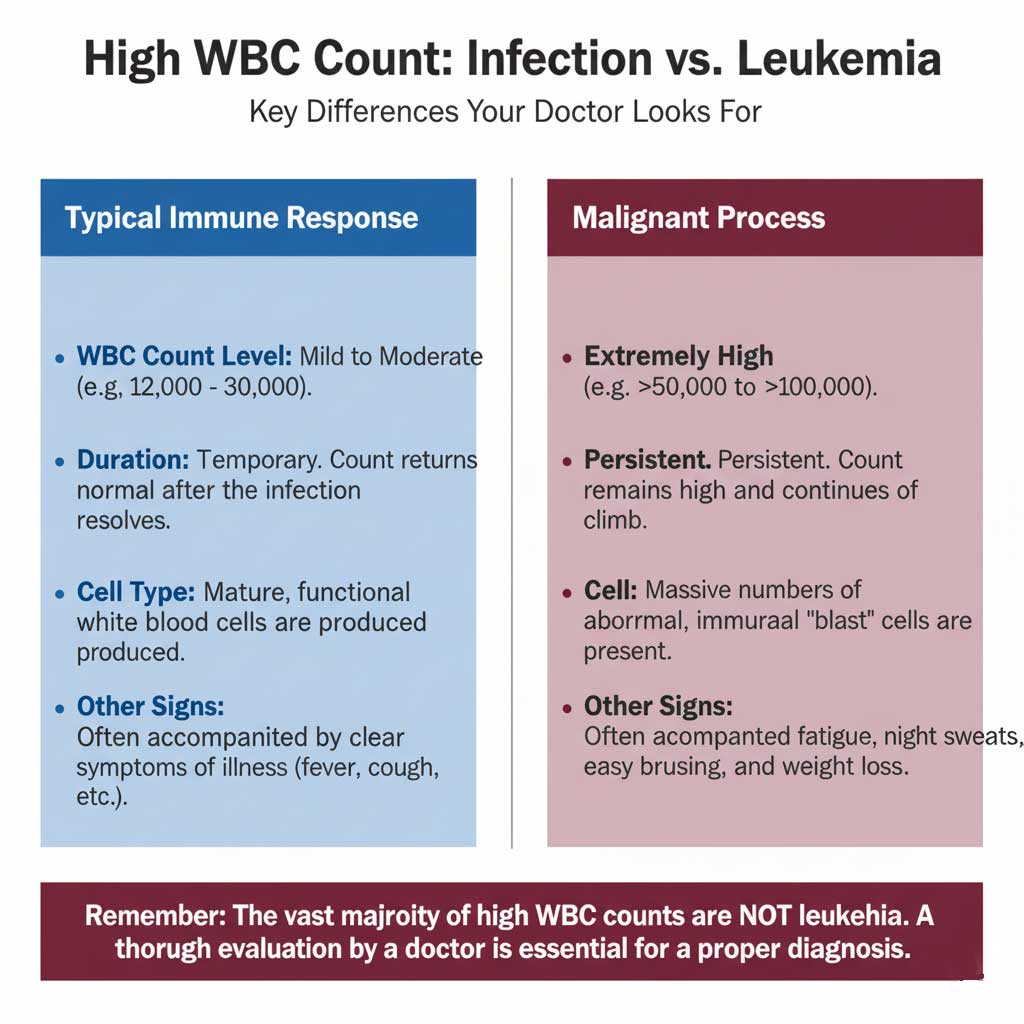
Distinguishing Infection from Cancer
The clues that point away from a simple infection and toward a more serious condition like leukemia are based on a few key factors:
- The Magnitude of the Count: The what level of white blood cells indicates leukemia is typically in a different ballpark. A WBC count 15000 is far more likely to be an infection or inflammation. In contrast, counts in acute leukemia are often extremely high, frequently exceeding 50,000 or 100,000 cells/mcL.
- The Persistence of the Count: A high white blood cell count due to an infection or stress is transient. As you recover, the count will return to the normal WBC range. A WBC count caused by leukemia is persistently high and will typically continue to rise over time.
- The Appearance of the Cells: In a normal immune response, the body produces mature, functional white blood cells. In leukemia, the bone marrow produces a massive number of abnormal, immature white blood cells known as “blasts.” These cells do not function properly and crowd out healthy cells.
- Accompanying Symptoms: While infections cause symptoms like fever and aches, the red flag symptoms for leukemia include persistent fatigue, unexplained weight loss, night sweats, bone pain, and easy bruising or bleeding.
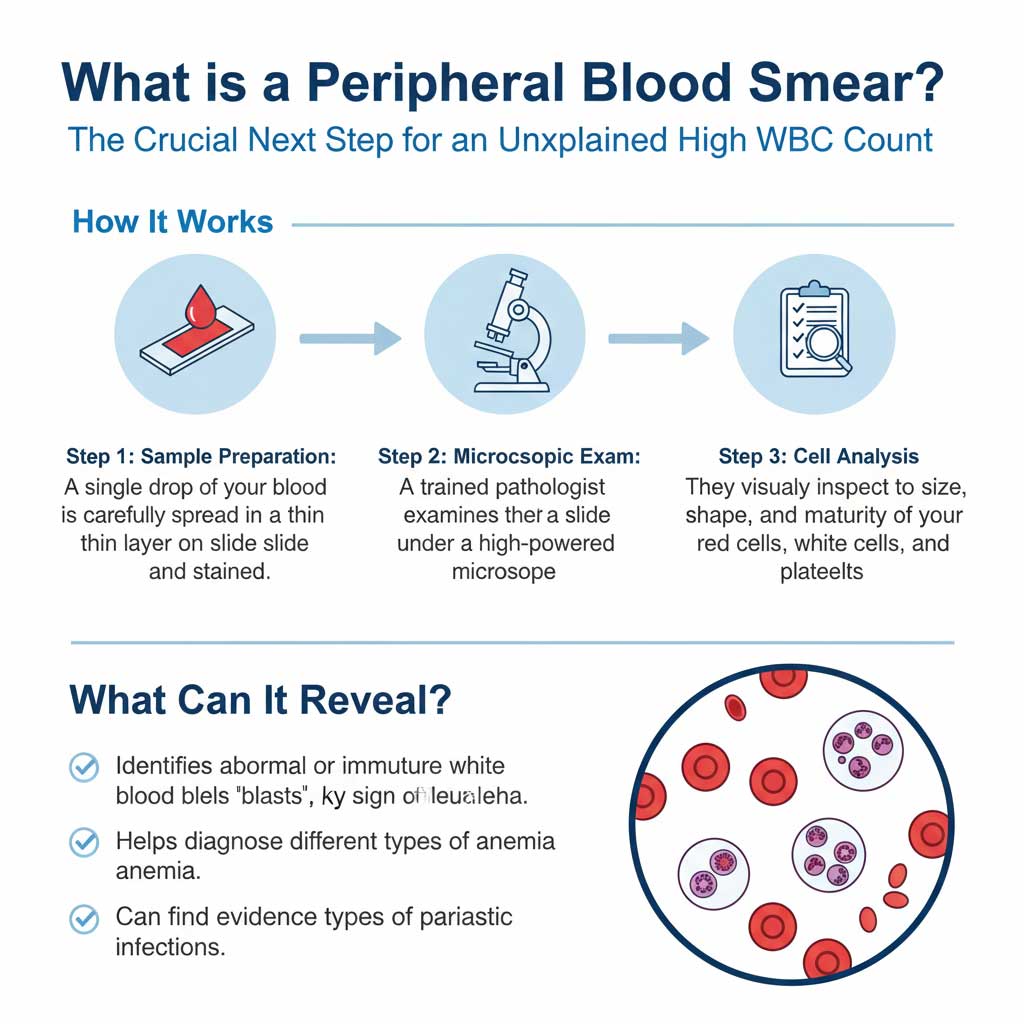
The Role of a Peripheral Blood Smear
If a blood cancer is suspected, the single most important next step is a peripheral blood smear. This is a simple but powerful test where a drop of your blood is spread on a glass slide, stained, and examined under a microscope by a trained pathologist. This allows them to visually inspect the size, shape, and maturity of your white blood cells. The presence of blasts on a peripheral blood smear is a key finding that points toward a diagnosis of acute leukemia.
The Diagnostic Process: What to Expect Next
If your blood test comes back with a high white blood cell count, here is the logical workflow you and your doctor will likely follow to determine the cause.
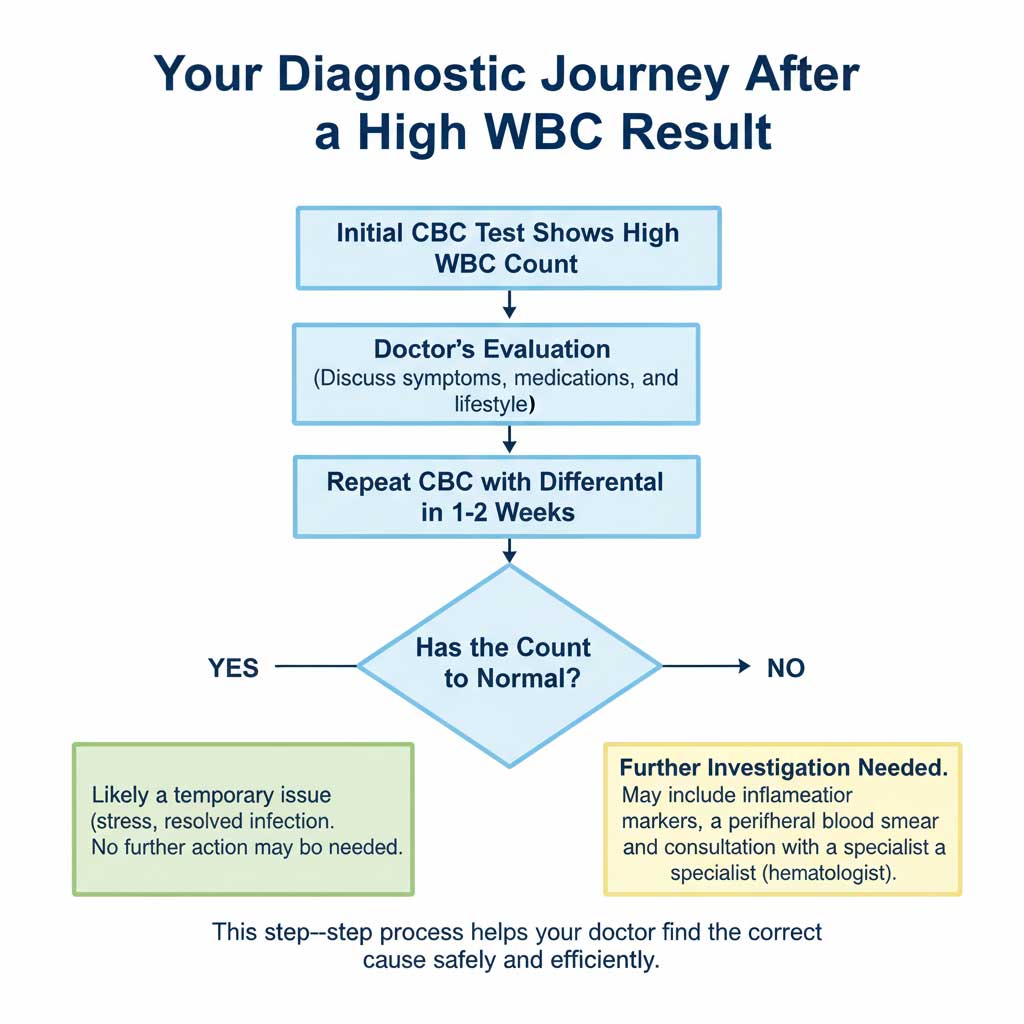
Step 1: Clinical Evaluation and History
The diagnostic process begins with a conversation. Your doctor will ask about:
- Any symptoms you are experiencing (fever, cough, pain, etc.).
- All medications you are taking, including over-the-counter drugs and supplements.
- Your lifestyle habits, such as smoking.
- Any recent illnesses, injuries, or significant stressors.
Step 2: Repeating the Test
Because a WBC count can be temporarily elevated, the first step is often to repeat the CBC with differential in a week or two. This helps determine if the leukocytosis was a transient spike or if it is a persistent issue that requires further investigation. You can easily order a follow-up CBC with Differential test online through BloodTestCenter.com to monitor your levels conveniently and prepare for your next doctor’s visit.
Step 3: Additional Blood Tests
If the count remains high, your doctor may order other blood tests to look for signs of inflammation, such as a C-reactive protein (CRP) or an Erythrocyte Sedimentation Rate (ESR).
Step 4: Advanced Testing (If Necessary)
If the cause is still not clear or if a serious condition is suspected, more advanced tests will be ordered. This is when the peripheral blood smear becomes critical. In the rare case that a blood cancer is strongly suspected, the definitive test is a bone marrow biopsy, which provides a direct sample of the blood-forming tissue for analysis.
Conclusion: Your Results are a Starting Point, Not a Final Diagnosis
Receiving a lab report with a high white blood cell count can be stressful, but it’s important to view it as a valuable piece of information, not a final verdict. In most cases, leukocytosis is simply a sign that your immune system is doing its job effectively. The most crucial clues lie in the magnitude of the count, whether it is persistent, and the results of your CBC with differential.
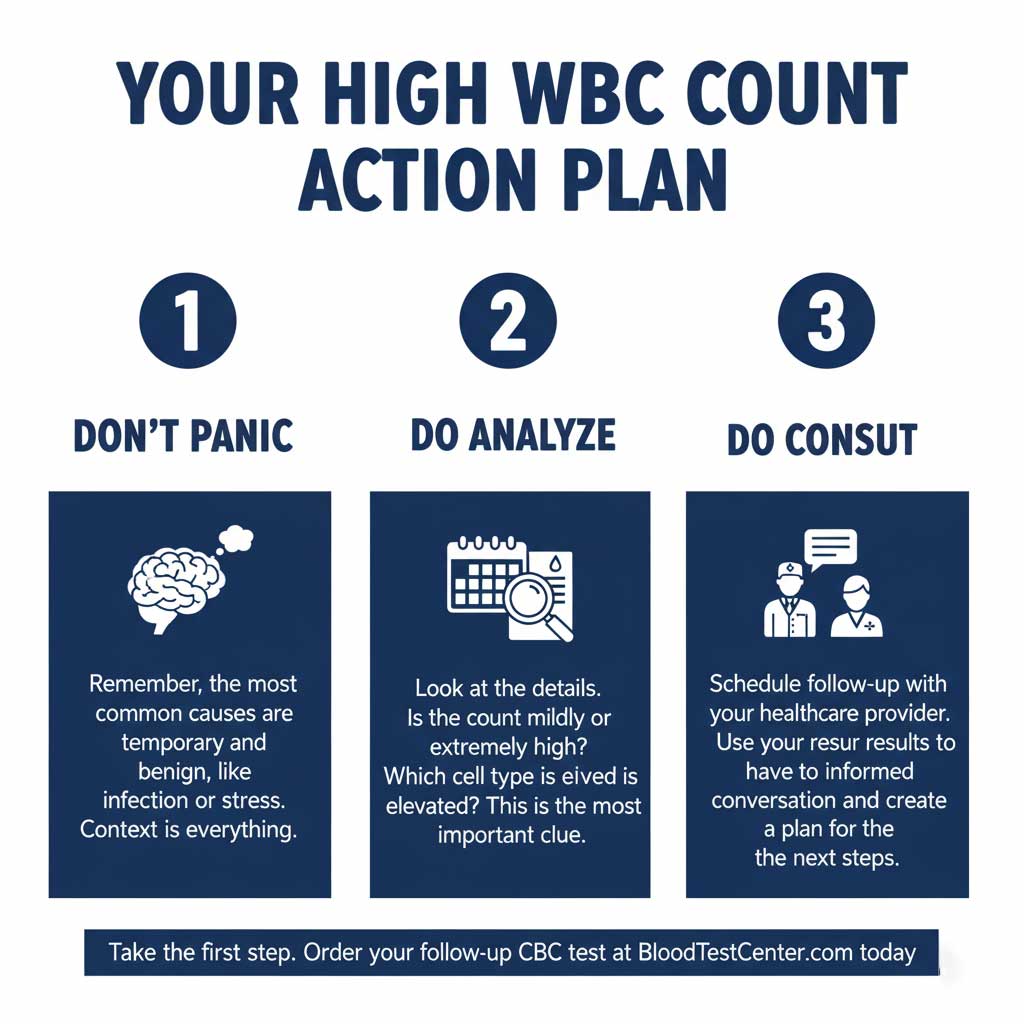
Your blood test results empower you to have a more informed, productive conversation with your healthcare provider. Don’t panic. Instead, use this information to take proactive steps. If you’re concerned about your levels or need a follow-up test, order your CBC with Differential at BloodTestCenter.com today and schedule a consultation with a healthcare professional to discuss your results.
Frequently Asked Questions (FAQ)
1. Is a WBC count of 12,000 or 15,000 considered dangerous?
A WBC count 12000 or a WBC count 15000 is considered a mild leukocytosis. It is not typically dangerous in itself but is a signal that your body is dealing with something, most commonly an infection or significant stress. It warrants a follow-up with your doctor to determine the cause.
2. How long does it take for a high WBC count to return to normal after an infection?
After a typical infection, your WBC count should begin to decrease as you recover and usually returns to the normal WBC range within one to two weeks after the infection has resolved.
3. Can anxiety or a panic attack cause a temporarily high WBC count?
Yes. The surge of stress hormones like adrenaline during a period of high anxiety or a panic attack can cause a rapid, temporary release of white blood cells into the bloodstream, leading to a transient high white blood cell count.
4. Can I have a high WBC count with no symptoms?
Absolutely. This is quite common. You might have a low-grade infection your body is fighting off without producing obvious symptoms, or the elevation could be due to a medication you’re taking or chronic inflammation from a condition like smoking. This is a key reason why routine blood work is so valuable.
5. What does a high WBC count mean during pregnancy?
A moderately high white blood cell count is completely normal and expected during pregnancy. The physiological stress of carrying a pregnancy naturally stimulates the immune system. Counts up to 15,000 cells/mcL or even slightly higher are considered normal in the second and third trimesters.
6. Can dehydration affect my WBC count?
Yes. Dehydration reduces the plasma (liquid) volume of your blood. This can make the cellular components, including white blood cells, appear more concentrated, leading to a falsely elevated WBC count. This is known as relative leukocytosis and resolves with proper hydration.
7. Are there foods or natural ways to lower a high WBC count?
The treatment for a high white blood cell count is to address the underlying cause. There are no specific foods or supplements that will directly lower the count. The best “natural” approach is to support your immune system by managing the root issue, whether that’s resolving an infection, reducing stress, or quitting smoking.
8. What is the difference between leukocytosis and leukemia?
Leukocytosis is the general medical term for a high WBC count from any cause (infection, stress, cancer, etc.). Leukemia is a specific type of cancer that is one of the possible—but much rarer—causes of leukocytosis. All patients with leukemia have leukocytosis, but very few patients with leukocytosis have leukemia.
9. My total WBC is normal, but my neutrophils are high. What does that mean?
This is called relative neutrophilia. If your total WBC count is within the normal range but the percentage of neutrophils is high (and the percentage of lymphocytes is low), it can still be a subtle sign of an early bacterial infection or inflammation. It’s a finding worth discussing with your doctor.
10. How accurate are the WBC results from labs like Labcorp and Quest Diagnostics?
The automated hematology analyzers used by major certified labs like Labcorp and Quest Diagnostics are extremely accurate and reliable for counting white blood cells. The chance of a significant lab error on a WBC count is very low.

