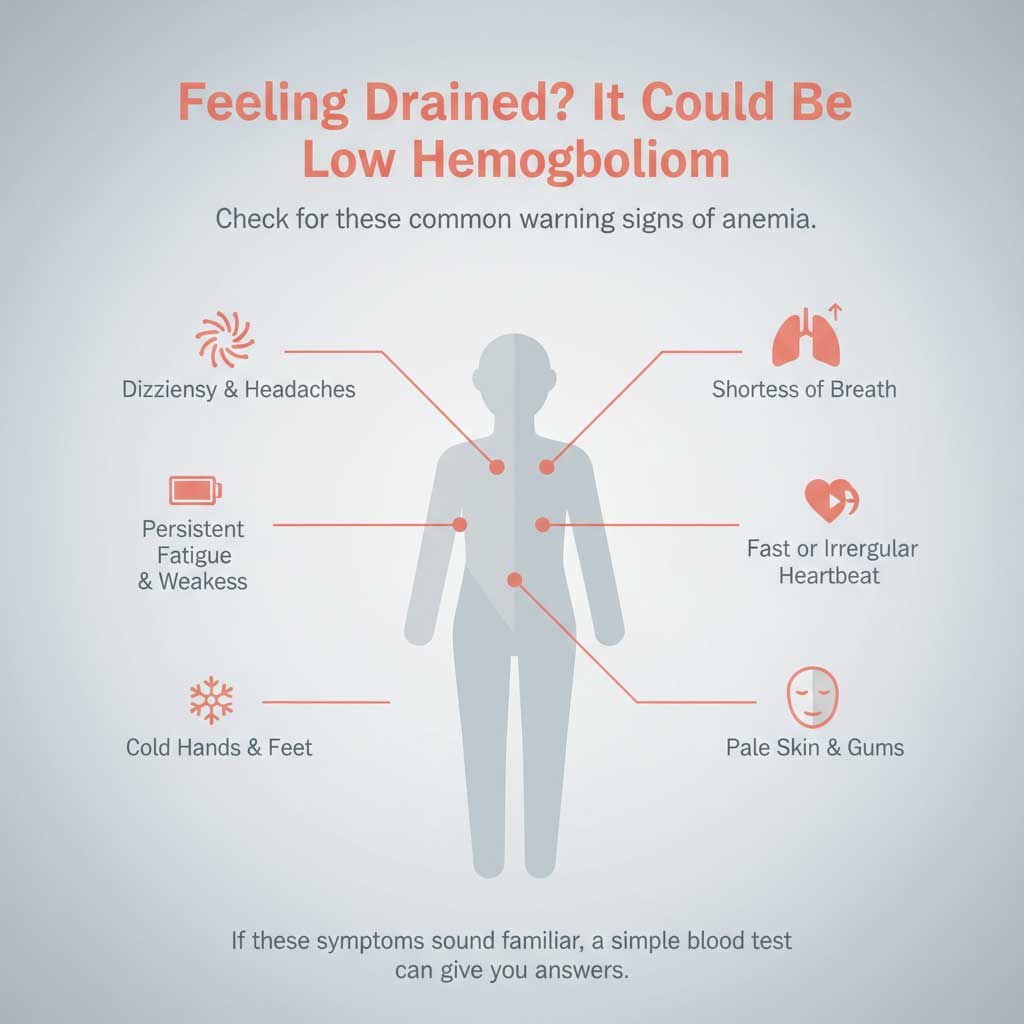
Do you suffer from a persistent, bone-deep fatigue that no amount of coffee can fix? Do you feel dizzy when you stand up too quickly or find yourself frustratingly short of breath after climbing a simple flight of stairs? These are more than just signs of a busy life; they are classic symptoms of low hemoglobin.
Table of Contents
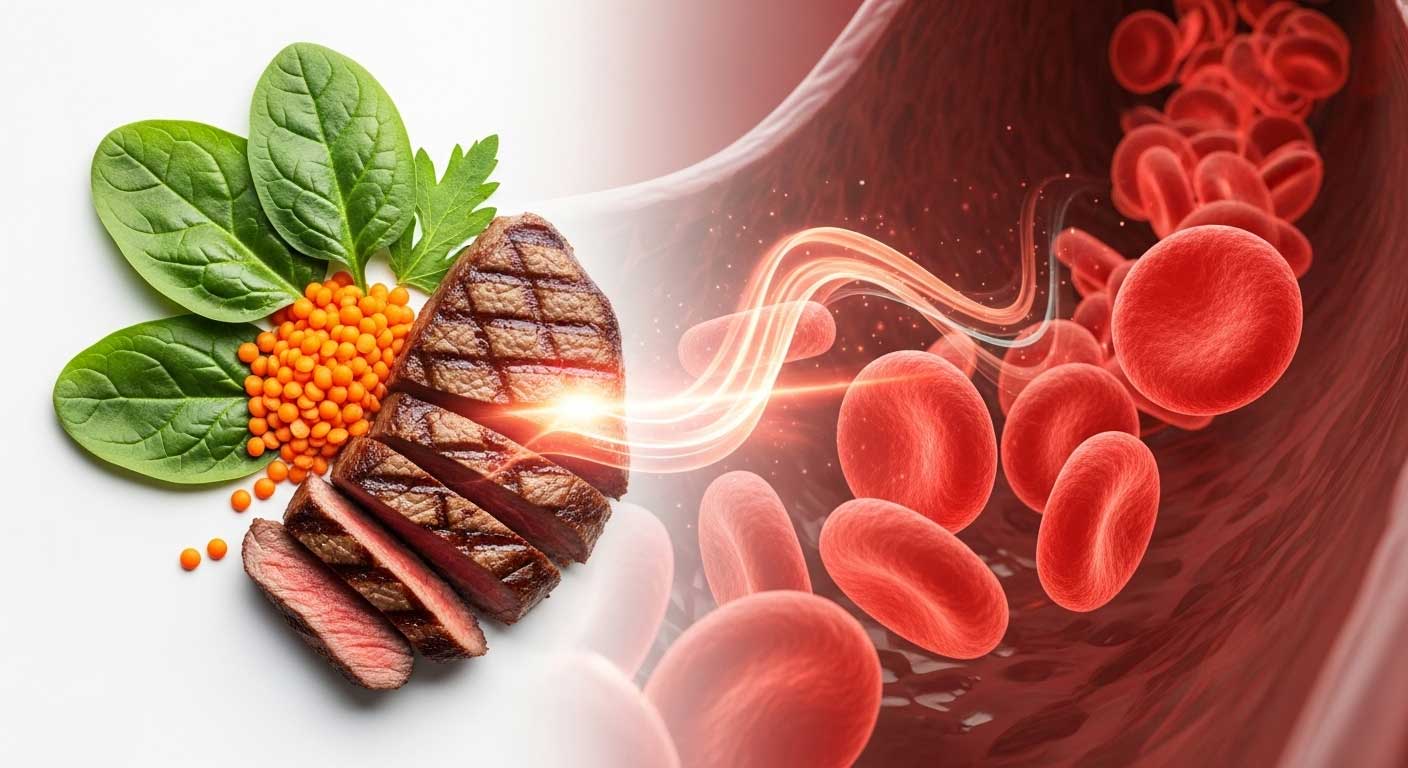
Hemoglobin is the body’s essential oxygen courier, and when its levels drop, a condition known as anemia can develop, leaving you feeling drained and unwell. This comprehensive, data-driven guide from BloodTestCenter.com will provide you with the most effective, science-backed strategies on how to increase hemoglobin quickly. While there are no magical “overnight” cures, a strategic combination of specific iron-rich foods, absorption-boosting vitamins, and, when necessary, targeted supplements, can significantly increase hemoglobin levels and help you reclaim your energy and vitality.
Understanding Hemoglobin: What It Is and Why You Need It
Before we can explore how to fix the problem, it’s essential to understand the basics of this vital component of your blood. This knowledge is the first step in having an informed conversation with your healthcare provider about how to increase hemoglobin.
What is Hemoglobin?
Hemoglobin (often abbreviated as Hb or Hgb) is an iron-containing protein found within your red blood cells. Its primary job is one of the most critical functions in the entire body. Think of each hemoglobin molecule as a dedicated delivery truck for oxygen. As your red blood cells pass through your lungs, hemoglobin latches onto oxygen molecules and transports them to every single cell, tissue, and organ, from your brain to your muscles. Without enough hemoglobin, this vital delivery service breaks down.
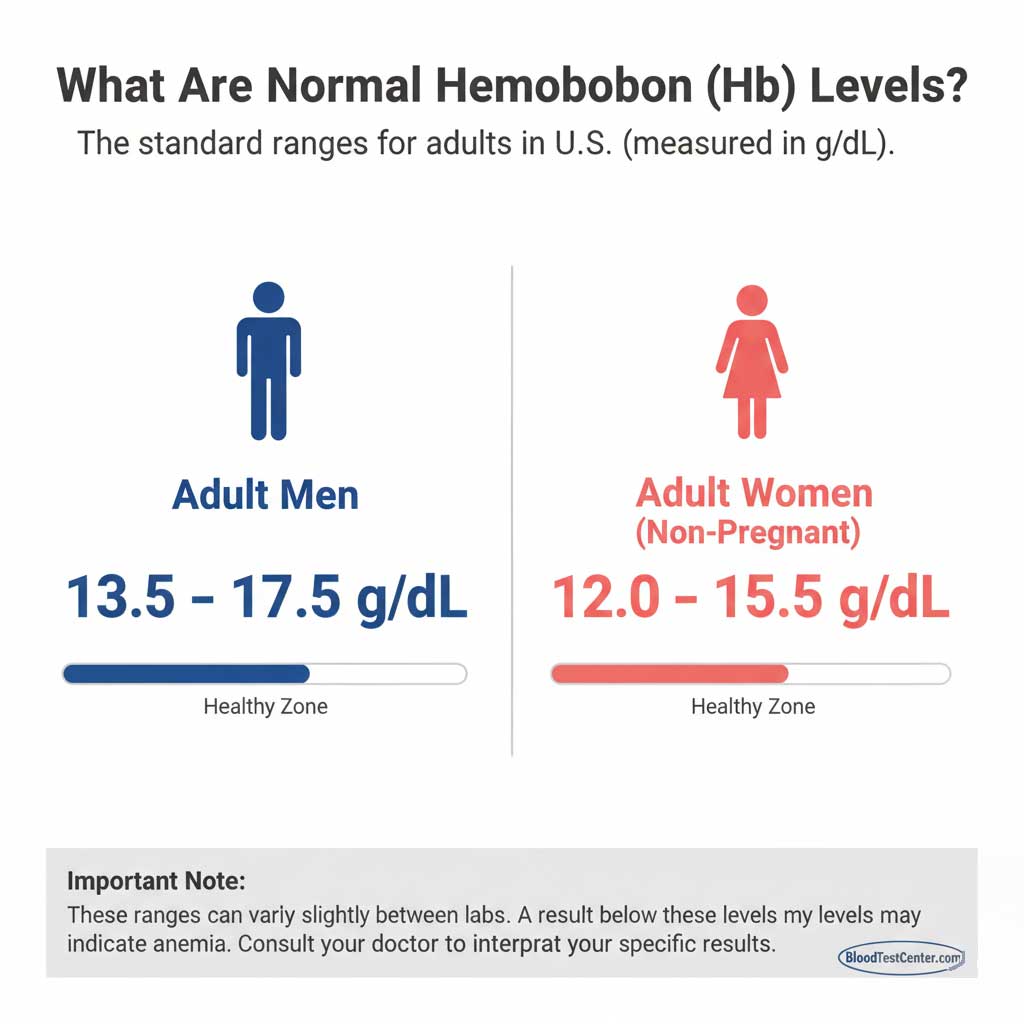
What Are Normal Hemoglobin Levels?
Your hemoglobin level is measured in grams per deciliter (g/dL) of blood. While the exact figures can vary slightly between different labs, the generally accepted normal hemoglobin levels for adults in the U.S. are:
- For Adult Men: 13.5 to 17.5 g/dL
- For Adult Women (non-pregnant): 12.0 to 15.5 g/dL
It’s important to note that these ranges can be different for children, and they naturally change during pregnancy to support the growing fetus. A result below these standard ranges typically indicates some degree of anemia.
What Causes Low Hemoglobin?
There are three main reasons why a person might develop low hemoglobin:
- Decreased Production: Your body isn’t making enough red blood cells or hemoglobin. This is most often caused by nutritional deficiencies, particularly a lack of iron, vitamin B12, or folate. It can also be due to chronic kidney disease or problems with the bone marrow.
- Increased Destruction: A condition called hemolytic anemia, where red blood cells are being destroyed faster than the body can produce them.
- Blood Loss: This can be obvious, such as from an injury or surgery, or it can be chronic and less apparent, like from heavy menstrual periods, ulcers, or other issues in the gastrointestinal tract.
The 3-Pronged Strategy for Rapid Hemoglobin Boosting
When you need to know how to increase hemoglobin quickly, it isn’t about a single magic food or pill. The most effective approach is a coordinated, three-pronged strategy that addresses iron intake, absorption, and the essential building blocks for red blood cells.
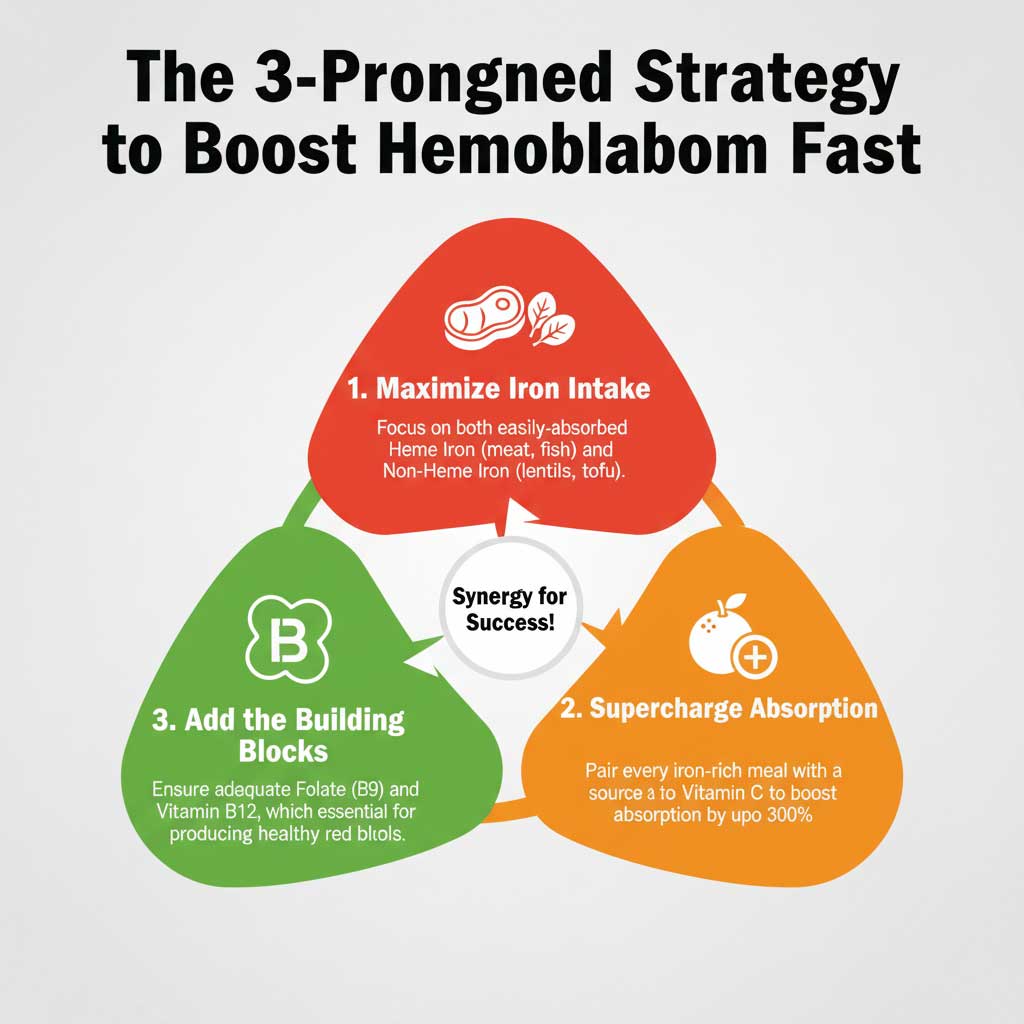
Pillar 1: Maximize Your Iron Intake
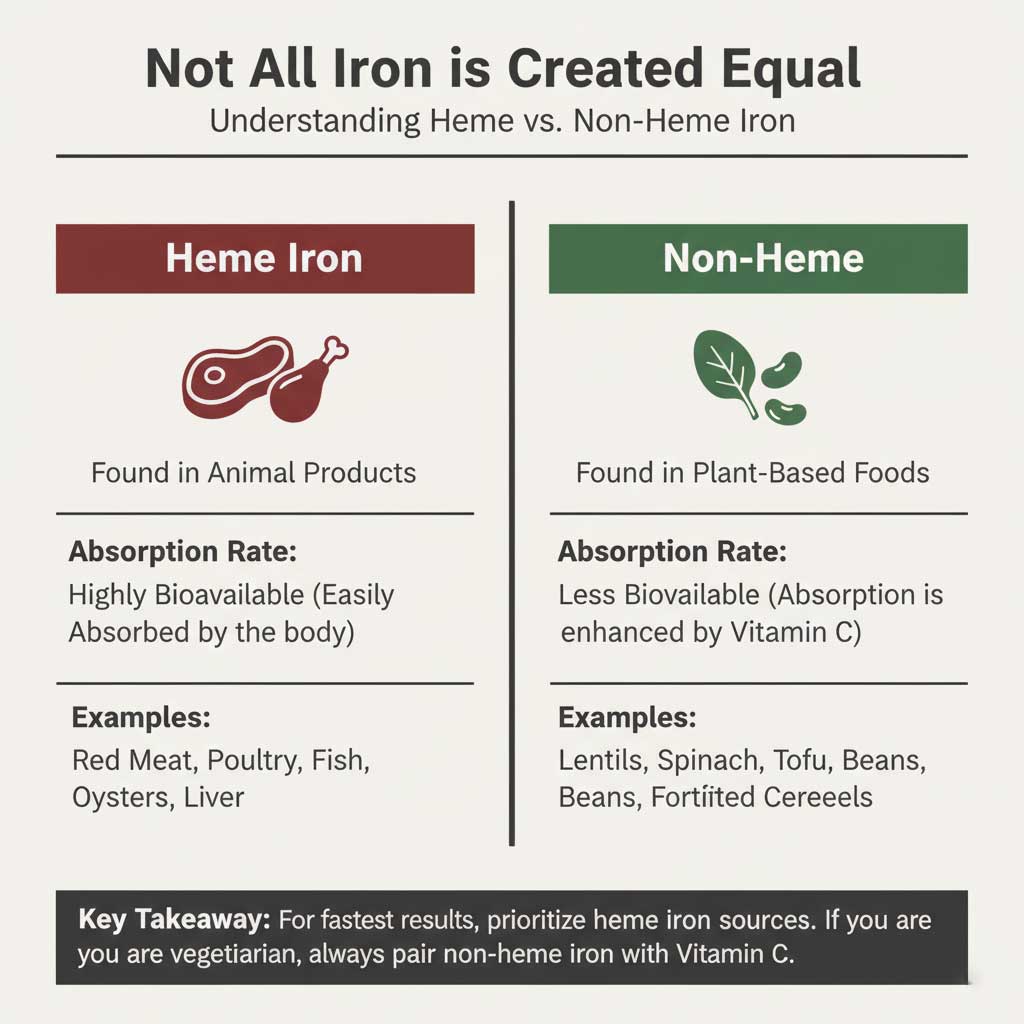
Iron is the central, non-negotiable component of the hemoglobin molecule. Increasing your dietary iron is the first and most important step. However, not all dietary iron is created equal.
- Heme Iron (The Fast Lane)Heme iron is found exclusively in animal products and is the most bioavailable form, meaning your body can absorb it very easily. If you are not a vegetarian, including sources of heme iron is one of the fastest ways to increase hemoglobin. Top sources include:
- Lean red meat (beef, lamb)
- Organ meats (especially beef liver)
- Poultry (chicken, turkey)
- Fish and shellfish (salmon, tuna, oysters)
- Non-Heme Iron (The Plant-Powered Path)Non-heme iron is found in plant-based foods. While it is less easily absorbed than heme iron, it is a crucial source for everyone, especially vegetarians and vegans. Top vegan iron sources and other plant-based options include:
- Legumes (lentils, chickpeas, kidney beans, black beans)
- Leafy greens (spinach, kale)
- Tofu and edamame
- Seeds (pumpkin seeds, sesame seeds)
- Iron-fortified breakfast cereals and breads
Pillar 2: Supercharge Your Iron Absorption with Vitamin C
This is perhaps the most important “hack” for boosting your iron levels, especially if you rely on plant-based sources. Vitamin C and iron absorption have a powerful synergistic relationship. Vitamin C captures non-heme iron and converts it into a form that your body can absorb much more easily.
- Data Point: Consuming a good source of vitamin C along with your non-heme iron source can increase iron absorption by as much as 300%.
- Practical Instances: This is easy to implement in your daily meals.
- Squeeze fresh lemon juice over a spinach salad.
- Add bell peppers (one of the best sources of Vitamin C) to a tofu stir-fry.
- Have a small glass of orange juice with your iron-fortified breakfast cereal.
- Incorporate tomatoes into your lentil soup or chili.
Pillar 3: Get the Essential Building Blocks – Folate & Vitamin B12
While iron gets most of the attention, it can’t build hemoglobin on its own. Think of iron as the main ingredient, but folate (Vitamin B9) and Vitamin B12 are the essential “construction workers” your bone marrow needs to build healthy, functional red blood cells. A deficiency in either of these vitamins can lead to anemia even if your iron intake is adequate.
- Folate (Vitamin B9): Found abundantly in leafy green vegetables, beans, peanuts, and enriched grains.
- Vitamin B12: Found almost exclusively in animal products (meat, fish, eggs, dairy). For vegans, it is essential to consume B12-fortified foods like nutritional yeast and plant-based milks, or to take a supplement.
Your Diet Action Plan: The Best Foods to Increase Hemoglobin
Putting this strategy into practice means making smart choices at the grocery store and in the kitchen. Here is a practical list of some of the best foods to increase hemoglobin.
| Category | Top Heme Iron Sources (Highly Absorbable) | Top Non-Heme Iron Sources (Plant-Based) | Top Vitamin C Boosters (Pair with Iron) |
| Meats & Poultry | Beef Liver: ~5 mg per 3 oz | Lentils: ~3.3 mg per 1/2 cup (cooked) | Bell Peppers: ~95 mg per 1/2 cup (raw) |
| Seafood | Oysters: ~8 mg per 3 oz | Spinach: ~3.2 mg per 1/2 cup (cooked) | Oranges: ~70 mg per medium fruit |
| Plant-Based Proteins | N/A | Tofu (firm): ~3 mg per 1/2 cup | Strawberries: ~49 mg per 1/2 cup |
| Legumes & Seeds | N/A | Chickpeas/Kidney Beans: ~2.5 mg per 1/2 cup | Broccoli: ~51 mg per 1/2 cup (cooked) |
| Fortified Foods | N/A | Fortified Breakfast Cereal: Varies, up to 18 mg per serving | Tomatoes: ~25 mg per medium fruit |
Foods and Drinks to Limit (The Iron Inhibitors)
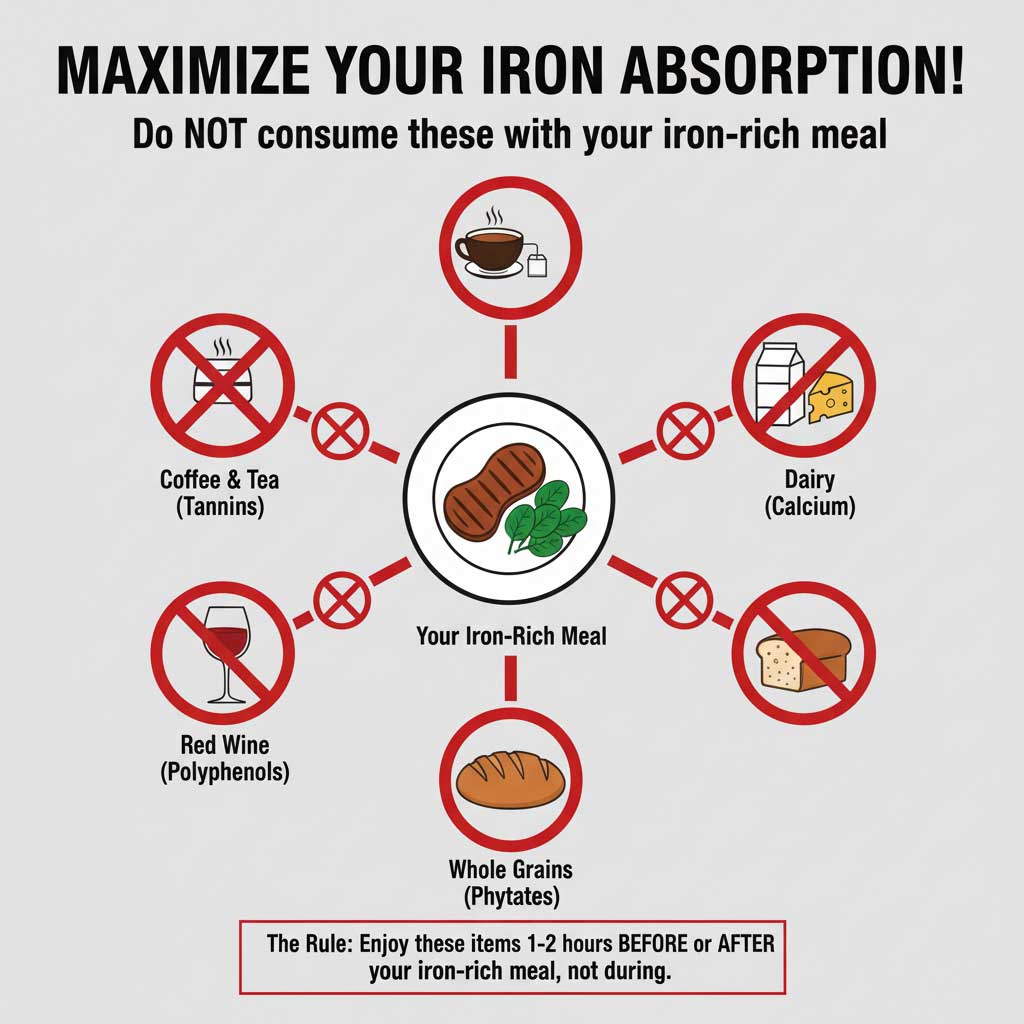
Just as important as what you eat is when you eat it. Certain compounds, known as iron inhibitors, can bind to iron in your gut and prevent it from being absorbed. One of the most common questions is, “does coffee affect iron absorption?” The answer is a definitive yes.
To maximize your efforts to increase hemoglobin, you should avoid consuming the following items at the same time as your iron-rich meal:
- Coffee and Tea: Contain compounds called tannins and polyphenols that severely block iron absorption.
- Dairy Products: The calcium in milk, cheese, and yogurt interferes with the absorption of both heme and non-heme iron.
- Foods High in Phytates: These include whole grains, legumes, and nuts.
Actionable Advice: This doesn’t mean you have to give up your morning coffee or favorite yogurt. Simply consume them at least one to two hours before or after your main iron-rich meal to give your body a clear window for absorption.
Iron Supplements: A Faster Path for Diagnosed Deficiencies
When dietary changes are not enough to correct a low hemoglobin level, or when the deficiency is significant, your doctor will likely recommend iron supplements for anemia.
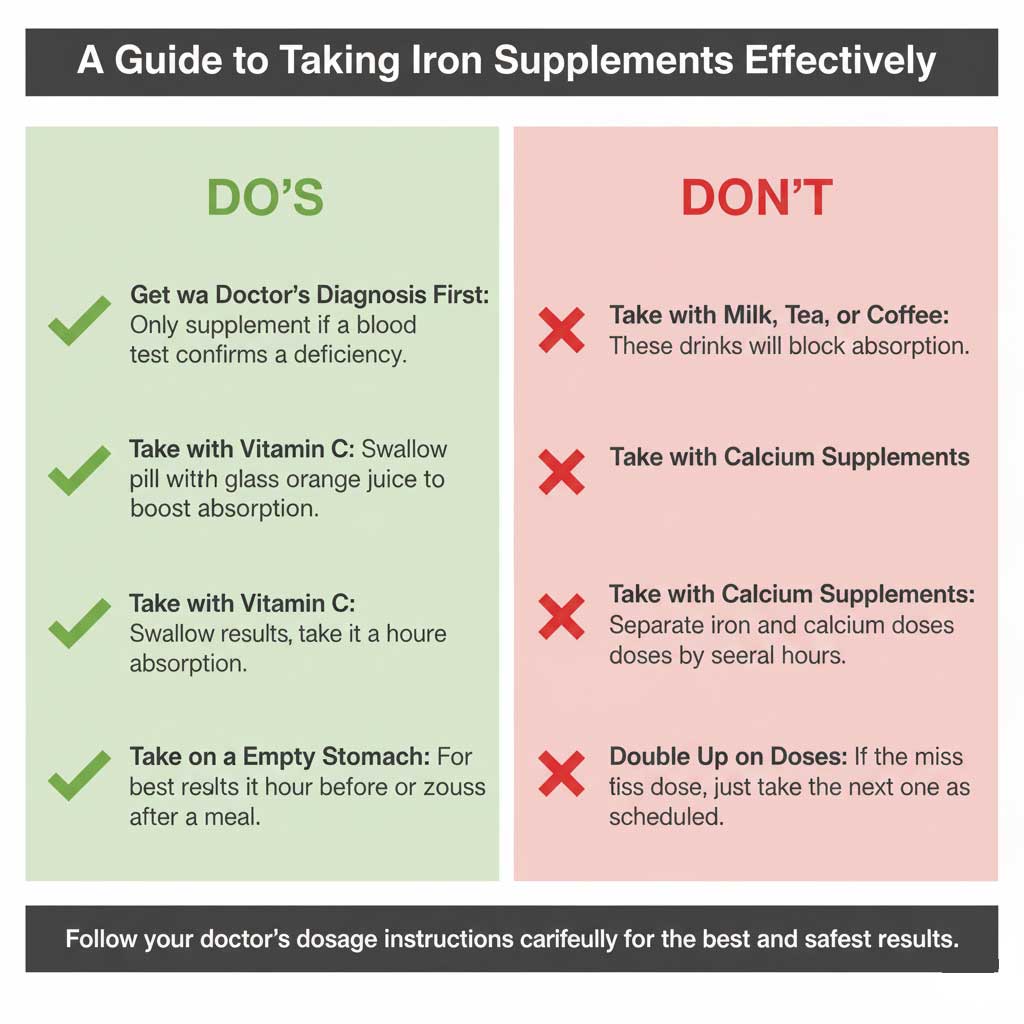
When Are Supplements Necessary?
It is crucial to only take iron supplements after you have confirmed a deficiency through a blood test from a provider like BloodTestCenter.com. Taking iron when you don’t need it can be harmful. Supplements are the right choice when your doctor determines that diet alone cannot replenish your iron stores quickly enough.
Choosing the Right Iron Supplement
The most common, effective, and cost-efficient form of over-the-counter iron is ferrous sulfate. Your doctor will recommend the appropriate dosage for you. To answer the question, “how much iron per day to increase hemoglobin?“, a typical therapeutic dose for treating iron-deficiency anemia in adults is around 150-200 mg of elemental iron daily. This is often split into two or three smaller doses throughout the day. This must be guided by a doctor.
Maximizing Absorption and Minimizing Side Effects
To get the most out of your supplement, take it on an empty stomach, about an hour before a meal, along with a source of vitamin C like a small glass of orange juice. However, iron supplements are notorious for causing side effects like nausea, stomach cramps, and constipation. If this happens, taking them with a small amount of food is better than stopping them altogether.
Realistic Timelines and Medical Interventions
One of the most common questions is “how long to increase hemoglobin?” It’s important to set realistic expectations.
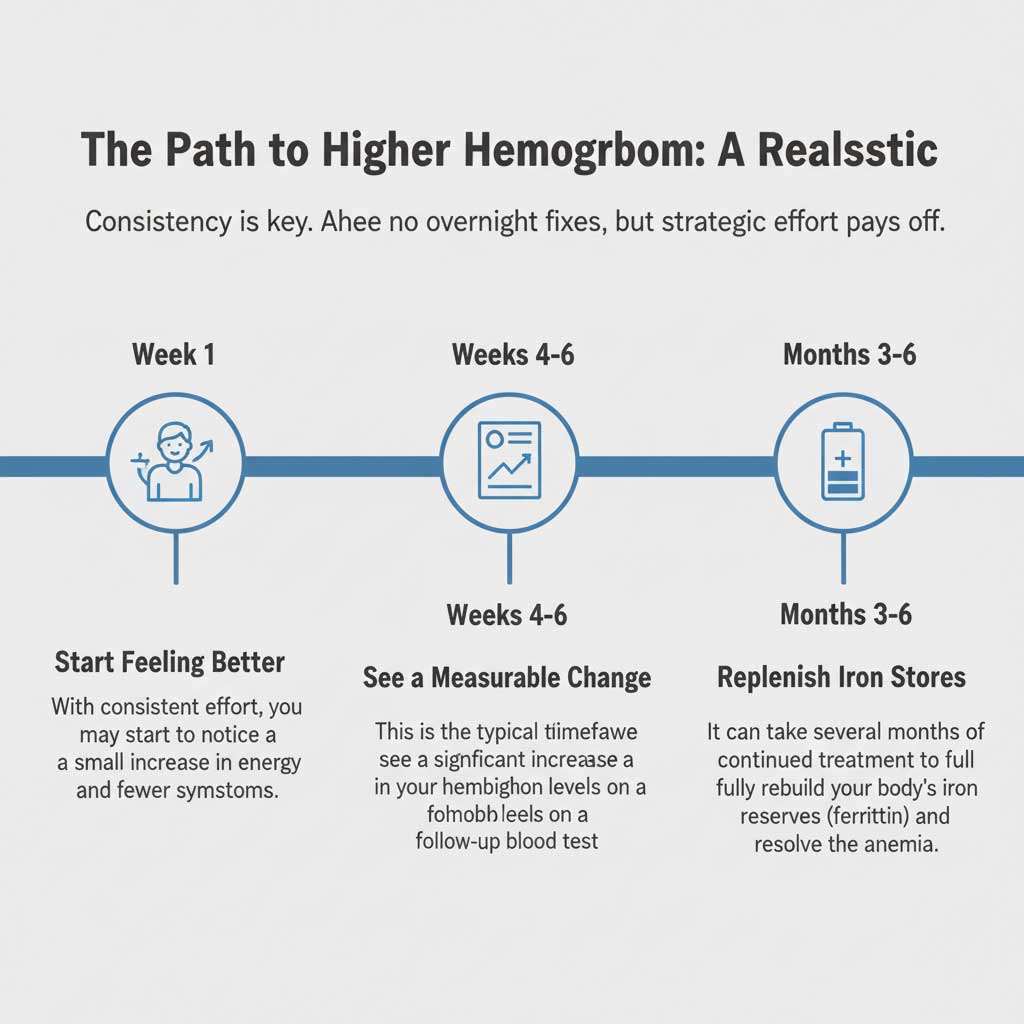
- Can you increase hemoglobin in a week? You can certainly start the process and may even begin to feel a bit better, but you will not see a full correction on your blood test in just one week.
- The Realistic Timeline: With consistent and aggressive dietary changes and supplementation, it typically takes 4 to 6 weeks to see a significant and measurable increase in your hemoglobin levels. The journey back to the normal hemoglobin levels is a marathon, not a sprint.
When Diet and Pills Aren’t Enough: The Fastest Medical Options
For cases of severe anemia or when oral iron isn’t being absorbed properly, doctors have more powerful tools.
- IV Iron Infusions: This is often the fastest way to recover from anemia without a transfusion. Iron is delivered directly into your bloodstream through an IV, bypassing the digestive system entirely. This results in a much quicker replenishment of iron stores.
- Blood Transfusions: This is an emergency or urgent intervention reserved for patients with critically low hemoglobin (typically below 7 or 8 g/dL) or those who have experienced significant and rapid blood loss. A transfusion provides an immediate increase in hemoglobin and oxygen-carrying capacity.
Conclusion: Take Control of Your Energy and Health
The journey to increase hemoglobin is a proactive and empowering step toward reclaiming your energy, mental clarity, and overall well-being. The strategy is clear: maximize your intake of iron-rich foods, supercharge absorption by pairing them with vitamin C while avoiding inhibitors like coffee and dairy, and ensure you have enough of the essential red blood cell “building blocks”—folate and Vitamin B12.
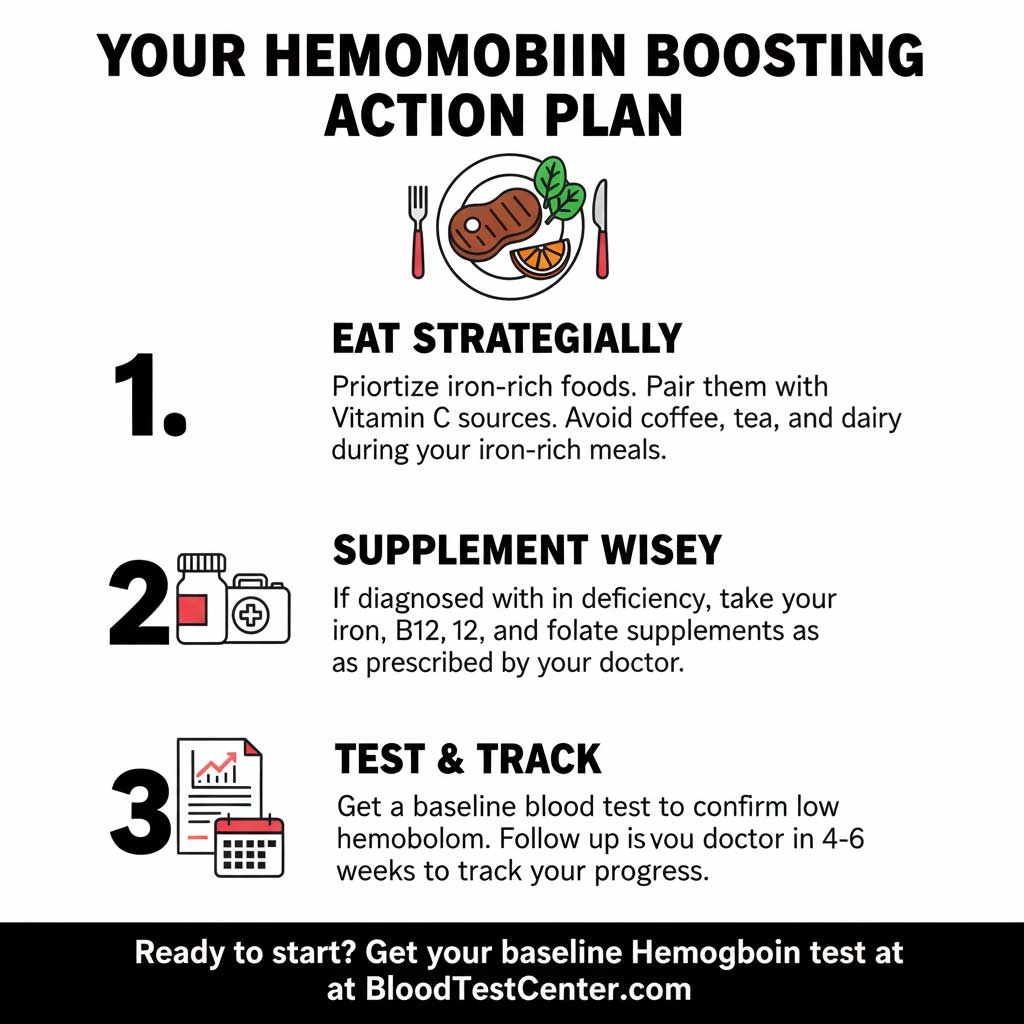
If you are experiencing the persistent symptoms of low hemoglobin, the first step is to get a clear diagnosis. Don’t guess, get tested. Order a Hemoglobin Test or a Complete Blood Count (CBC) from BloodTestCenter.com today. With an accurate result in hand, you can work with your healthcare provider to build a powerful action plan using the strategies in this guide and start your journey back to optimal health.
Frequently Asked Questions (FAQ)
1. What are the first signs that my hemoglobin is increasing?
The first signs are usually a noticeable improvement in your symptoms. You may feel a gradual increase in your energy levels, less shortness of breath during activities, and a reduction in dizziness. Your skin may also regain some of its color.
2. Is drinking beetroot juice a fast way to increase hemoglobin?
Beetroot is rich in folate and other nutrients, but it is not a particularly high source of iron. While it can be part of a healthy diet to support red blood cell production, relying on it alone is not a fast or effective strategy to correct an iron deficiency.
3. Can anemia be cured permanently?
If the anemia is caused by a nutritional deficiency (like low iron) that is corrected and maintained through diet and/or supplements, it can be considered cured. If the anemia is caused by a chronic disease or a genetic condition, it may require ongoing management.
4. How much iron is too much? Can I overdose on supplements?
Yes, it is possible to get too much iron, a condition called iron overload or hemochromatosis. This is why it is critical to only take iron supplements for anemia under the guidance of a doctor after a confirmed deficiency.
5. How often should I get my hemoglobin levels re-tested when treating a deficiency?
Your doctor will typically re-test your hemoglobin and iron levels (specifically ferritin) about 4 to 6 weeks after you start treatment to see if the plan is working. Follow-up tests will continue periodically until your levels are back in the normal hemoglobin levels.
6. Does exercise help increase hemoglobin?
Yes, regular moderate to intense exercise can help increase hemoglobin. When you exercise, your body’s demand for oxygen increases. This signals your body to produce more red blood cells and hemoglobin to meet that demand.
7. Why is my hemoglobin low even though I eat a lot of iron?
This could be due to several reasons. You might have an absorption issue (like celiac disease or IBD), you might be consuming iron inhibitors (like coffee or tea) with your meals, or your body’s need for iron might be higher than your intake (due to things like heavy menstrual bleeding or pregnancy).
8. Is it common to have low hemoglobin during pregnancy?
Yes, it is very common. During pregnancy, a woman’s blood volume increases significantly to support the baby, which dilutes the red blood cells. This, combined with the baby’s own need for iron, often leads to a mild physiological anemia.
9. How can I quickly increase hemoglobin after donating blood?
After donating blood, focus on the 3-pronged strategy immediately. Eat an iron-rich meal paired with vitamin C, ensure you are well-hydrated, and avoid inhibitors. Your body’s iron stores (ferritin) will be used to create new red blood cells, a process that takes several weeks.
10. What’s the difference between hemoglobin and ferritin?
Hemoglobin is the functional iron-protein in your red blood cells that is actively carrying oxygen. Ferritin is the protein that stores iron in your body’s cells, acting as your iron savings account. Low ferritin is the first sign of iron deficiency, often appearing long before your hemoglobin level drops.