For millions of Americans, a daily low-dose aspirin has become a familiar ritual, a small pill taken with the hope of protecting their heart. Given its well-known benefits for the cardiovascular system, a logical and incredibly common question arises: does aspirin lower blood pressure, too? It seems like a simple question, but the answer is complex, surrounded by decades of conflicting online information, outdated advice, and genuine scientific debate.
Table of Contents
This confusion can lead to potentially unsafe health decisions. Many people with hypertension wonder if they should be taking aspirin for high blood pressure in addition to their prescribed medications, while others might consider it a “natural” alternative.
This article will provide a clear, definitive, and science-backed answer to that question. We will dive deep into the latest and most reliable clinical trials, meta-analyses, and official U.S. medical guidelines to explain what the evidence truly says about low-dose aspirin blood pressure effects. We’ll uncover its real (and very limited) role, highlight the one critical exception where it’s recommended, and detail the significant risks that come with this everyday medication.
Aspirin and Blood Pressure: What the Major Studies Conclude
When we want to know if a medication works for a specific condition, we look at the highest quality scientific evidence available. For aspirin and its effect on blood pressure, the conclusion from large-scale research is surprisingly clear.
The Big Picture: Does Aspirin Work for Hypertension?
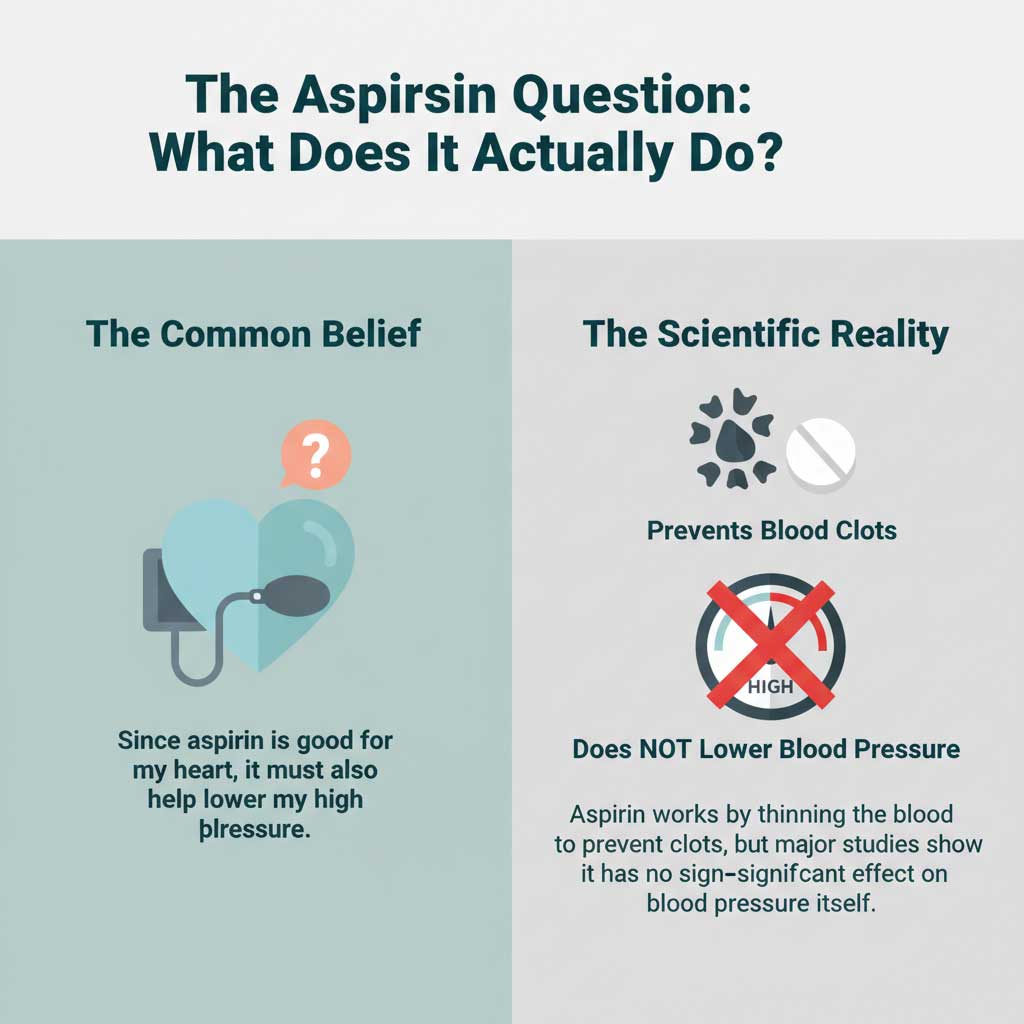
Let’s get straight to the point: The overwhelming scientific consensus today is that aspirin is not an effective treatment for lowering blood pressure. It does not provide a meaningful reduction in blood pressure for the vast majority of people with hypertension.
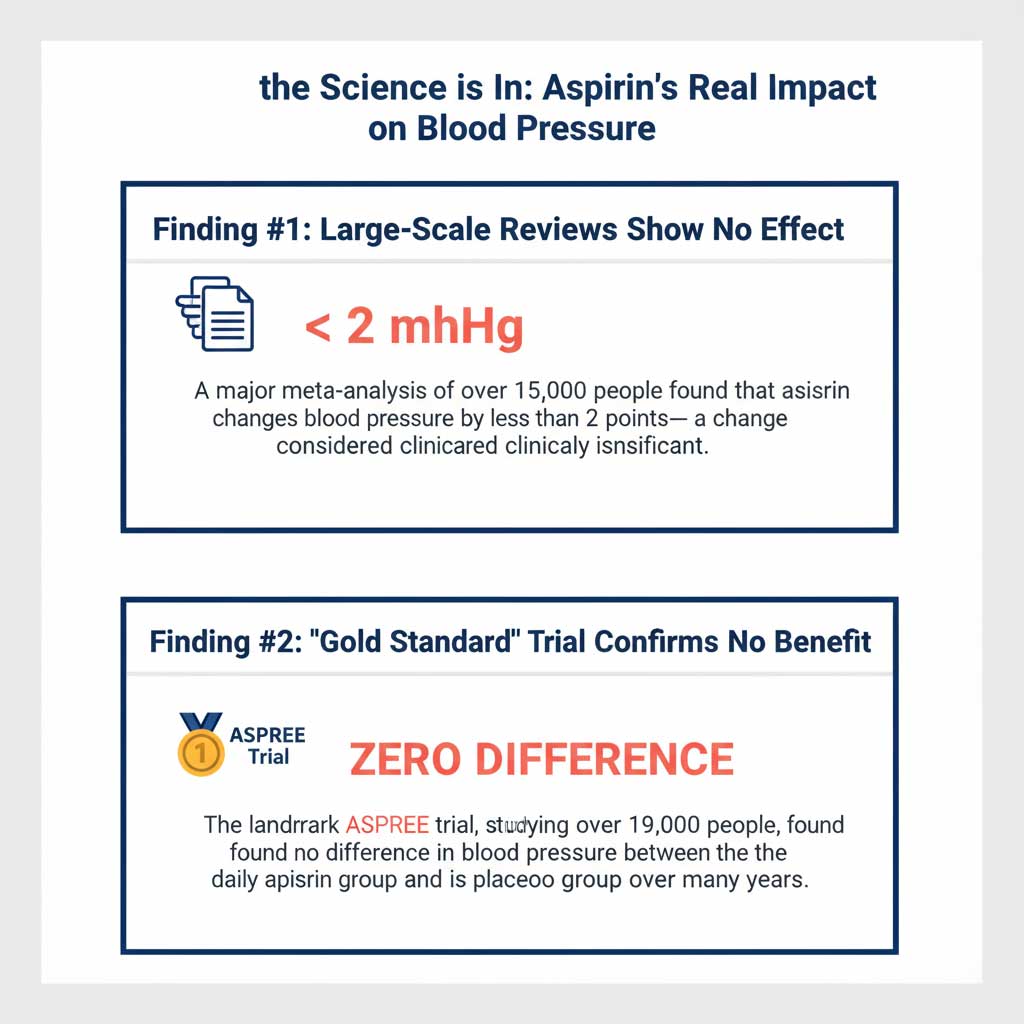
To understand why this is the accepted conclusion, we look at meta-analyses, which are powerful studies that combine the results of many individual clinical trials to get a more reliable answer. A major meta-analysis published in the prestigious journal Hypertension did exactly this. After reviewing 23 high-quality randomized controlled trials that included over 15,000 participants, the researchers found that daily aspirin use had no statistically significant effect on either systolic vs diastolic blood pressure.
While some individual studies showed tiny fluctuations, the overall effect was a change of less than 1-2 mmHg—an amount so small that it is not considered clinically significant for managing high blood pressure.
The Landmark ASPREE Trial
Further cementing this conclusion is the landmark ASPREE (Aspirin in Reducing Events in the Elderly) trial. This “gold standard” of clinical research was a massive, multi-year study involving over 19,000 older adults in the U.S. and Australia. It was designed to determine the true risks and benefits of daily low-dose aspirin in a healthy, older population.
One of the key things the researchers monitored was blood pressure. The verdict was unambiguous: there was no difference in blood pressure levels between the group taking 100 mg of aspirin daily and the group taking a placebo. This powerful evidence from a massive, well-designed trial is a primary reason why the answer to “does aspirin lower blood pressure?” is a firm no from the medical community.
The “Bedtime Aspirin” Debate: A Myth That Won’t Go Away
If you’ve searched online about aspirin for high blood pressure, you’ve likely come across the theory that the timing of the dose matters. This is one of the most persistent and confusing topics in the discussion.
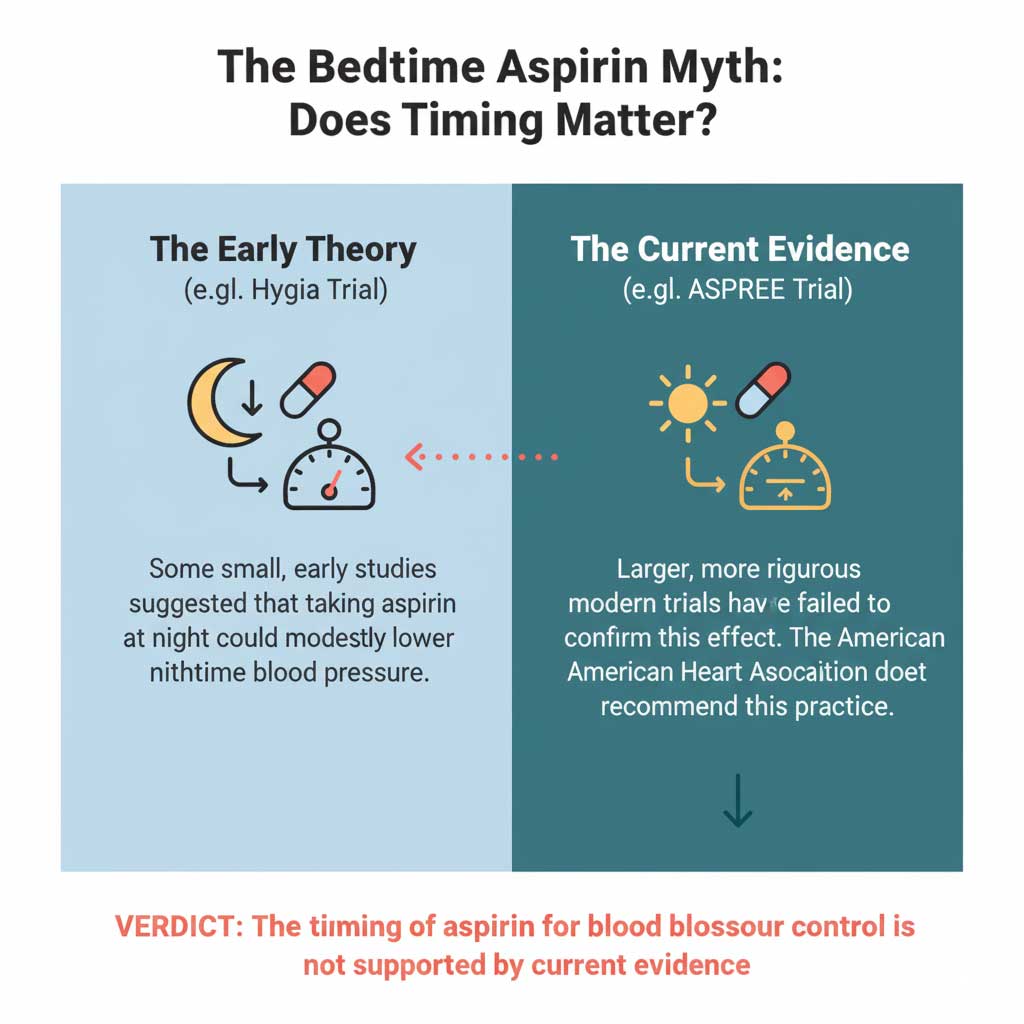
The Theory of Chronotherapy and Nighttime Blood Pressure
The idea is based on a concept called chronotherapy—the principle that a medication’s effect can change based on when you take it. Normally, a person’s blood pressure naturally dips during sleep. However, some people with hypertension are “non-dippers,” meaning their nighttime blood pressure stays elevated, which is a significant risk factor for heart attacks and strokes.
The Early Studies (Hygia Trial)
The theory that aspirin at bedtime for blood pressure could be beneficial gained traction from some earlier, smaller studies, most notably the Hygia Chronotherapy Trial. This study suggested that taking a low-dose aspirin at night, rather than in the morning, resulted in a modest but statistically significant drop in blood pressure, particularly during sleep. This finding was exciting and is the source of much of the ongoing confusion.
The Rebuttal from Larger, Modern Trials
While the bedtime theory was intriguing, science requires that findings be replicated in larger, more rigorous studies to be considered proven. In the case of bedtime aspirin, this has not happened.
Major, high-quality trials, including the aforementioned ASPREE trial aspirin study, specifically looked at this question and failed to replicate the results. They found no significant difference in blood pressure regardless of when the aspirin was taken. Because of this conflicting and weak evidence, the American Heart Association aspirin guidelines and other major medical bodies do not support the practice of taking aspirin at night to control blood pressure.
Aspirin for Blood Pressure vs. Heart Disease: A Summary of U.S. Guidelines
| Medical Use Case | Does Aspirin Help? | What the Science Says | Official U.S. Guideline (e.g., USPSTF, AHA) |
| General Blood Pressure Control | No | Large meta-analyses and trials (like ASPREE) show no clinically significant effect on systolic or diastolic blood pressure. | Not Recommended: No major U.S. guideline recommends aspirin for high blood pressure treatment. Standard antihypertensive medications should be used. |
| Primary Prevention of Heart Attack/Stroke | Only for a Select Group | Can reduce the risk of a first heart attack or stroke, but this benefit must be weighed against a significant bleeding risk. | Limited Recommendation (USPSTF): Consider for adults aged 40-59 with a ≥10% 10-year CVD risk who are not at high risk for bleeding. Recommend AGAINST starting in adults aged 60+. |
| Secondary Prevention of Heart Attack/Stroke | Yes, Generally Recommended | For patients who have already had a heart attack or stroke, aspirin is proven to significantly reduce the risk of a future event. | Strongly Recommended: Considered standard of care for most patients with established cardiovascular disease, unless contraindicated. |
| Prevention of Preeclampsia | Yes, for High-Risk Pregnancies | Clinical trials show low-dose aspirin significantly reduces the risk of developing this serious high blood pressure disorder during pregnancy. | Strongly Recommended (USPSTF & ACOG): Recommends 81 mg aspirin daily after 12 weeks of gestation for pregnant women at high risk for preeclampsia. |
The One Proven Exception: Aspirin for Preeclampsia Prevention
After establishing that aspirin is not a treatment for general hypertension, it is crucial to highlight the one specific and life-saving exception where it is strongly recommended for a high blood pressure condition.
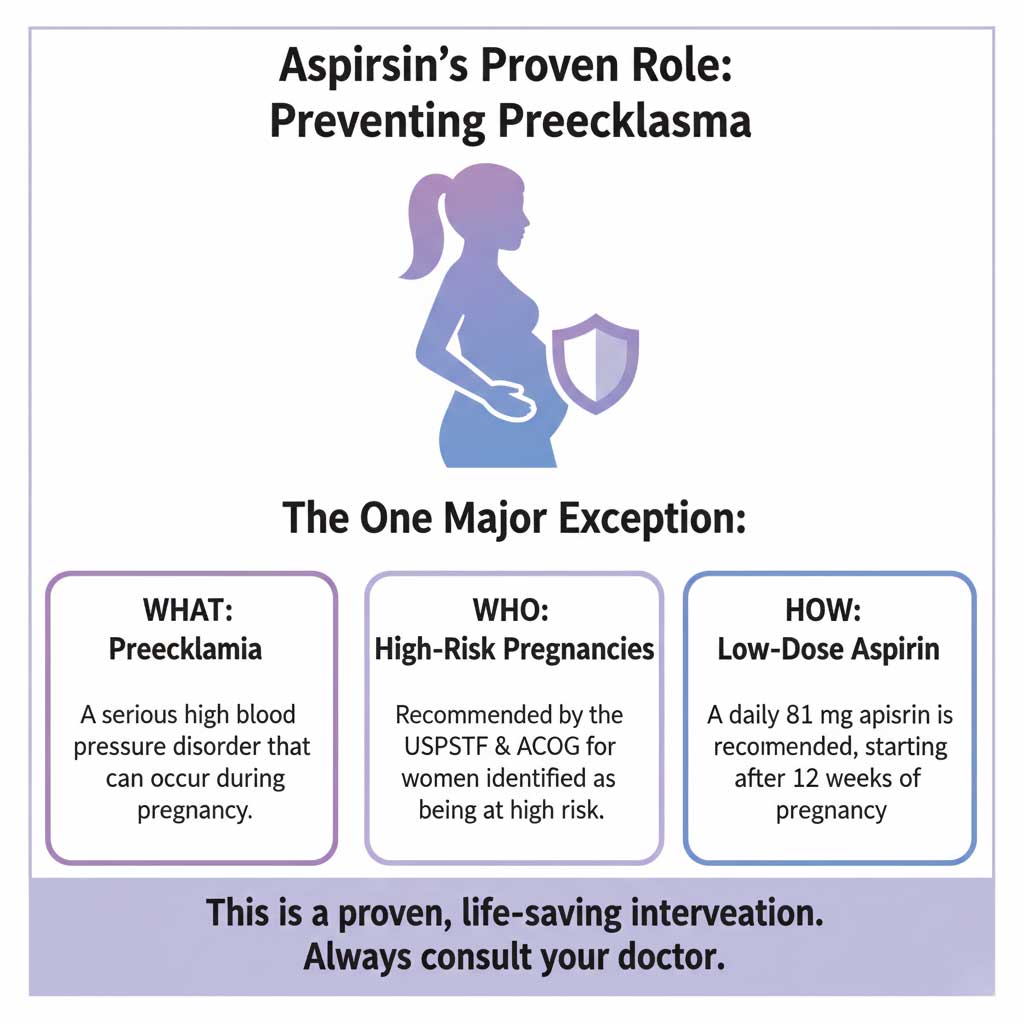
The Life-Saving Role of Aspirin in High-Risk Pregnancies
Preeclampsia is a serious and dangerous high blood pressure disorder that can develop during pregnancy, typically after 20 weeks of gestation. It can cause severe complications for both the mother (such as organ damage and seizures) and the baby (such as poor growth).
For women who are identified as being at high risk for developing this condition, daily low-dose aspirin is a proven preventive measure. This is the only hypertensive condition where the evidence for using aspirin is clear and overwhelming.
What the Official Guidelines Say
The recommendations from the top medical authorities in the United States are unified and direct.
- Instance: Both the U.S. Preventive Services Task Force (USPSTF) and the American College of Obstetricians and Gynecologists (ACOG) strongly recommend aspirin for preeclampsia prevention in high-risk pregnancies.
- The Regimen: The specific recommendation is for a low-dose aspirin (81 mg), often referred to as “baby aspirin,” to be taken daily. Treatment should begin after 12 weeks of gestation. This is a critical, evidence-based intervention that has been shown to significantly reduce the incidence of preeclampsia and improve outcomes for mothers and babies.
The Real Role of Aspirin: Heart Disease Prevention (and Its New Limits)
If aspirin doesn’t lower blood pressure, why do so many people with high blood pressure take it? The answer is that they are taking it to manage a different, though related, problem: the risk of heart attack and stroke.
Shifting from Blood Pressure to Cardiovascular Risk
The primary medical use for daily low-dose aspirin is for aspirin for heart attack prevention. It works not by affecting blood pressure, but by acting as a mild blood thinner. It makes platelets—the tiny cells that form blood clots—less “sticky.” This helps prevent the formation of dangerous clots that can block arteries and cause a heart attack or an ischemic stroke.
The New, More Cautious USPSTF Aspirin Guidelines
For decades, many Americans took a daily aspirin as a sort of “vitamin for the heart.” However, our understanding of the risk-benefit balance has evolved, and the official guidelines have become much more restrictive.
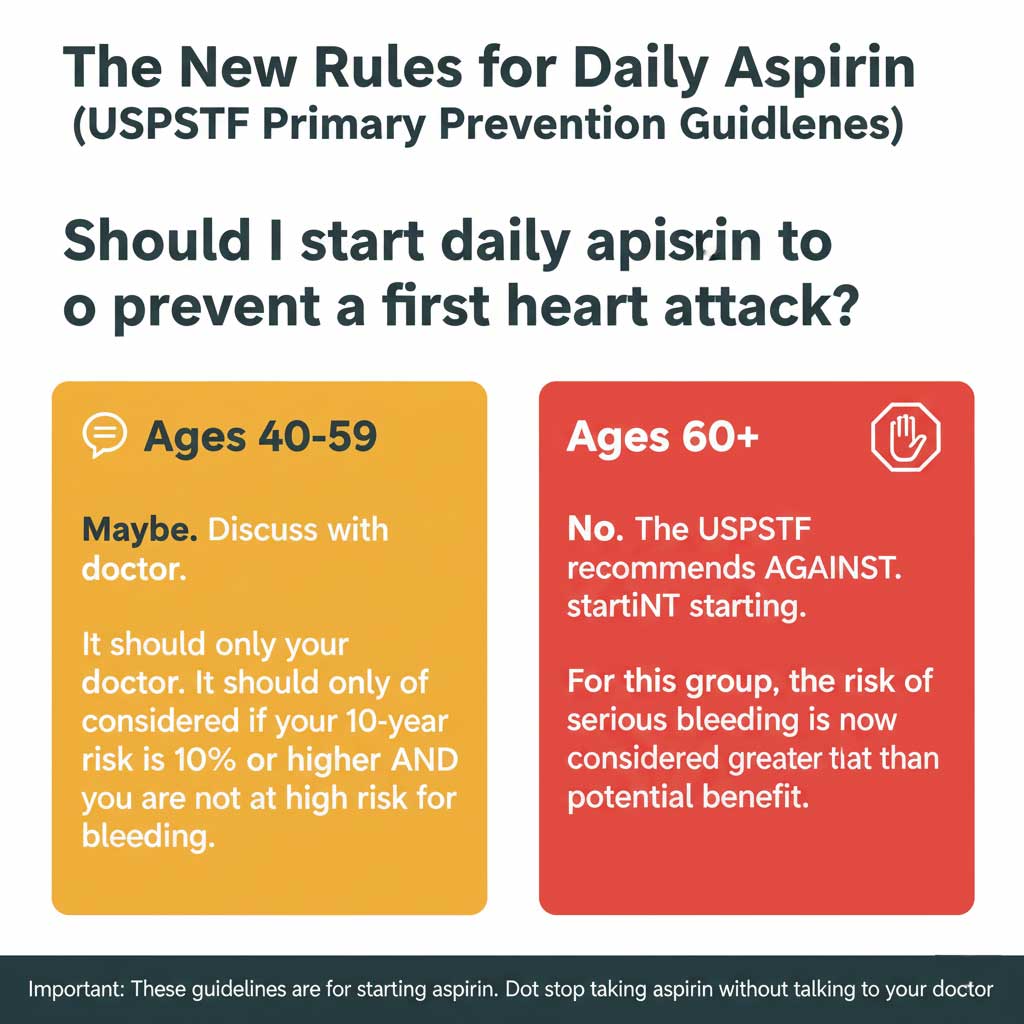
The USPSTF aspirin guidelines, which are the gold standard for preventive medicine in the U.S., were significantly updated in recent years. The current recommendations for primary prevention (preventing a first heart attack or stroke) are now very specific:
- Adults Aged 40-59: Daily low-dose aspirin should only be considered for individuals in this age group who have a 10-year cardiovascular disease (CVD) risk of 10% or higher AND are not at an increased risk for bleeding. The decision to start aspirin should be an individual one, made in close consultation with a doctor.
- Adults Aged 60 and Older: The USPSTF now recommends AGAINST starting daily aspirin for primary prevention in this age group. Research, including the ASPREE trial, has shown that for older adults, the risk of serious bleeding from aspirin outweighs the potential benefit in preventing a first heart attack.
It’s crucial to note that these guidelines are for starting aspirin. If you are already taking daily aspirin under a doctor’s recommendation, you should not stop without consulting them first.
The Serious Downsides: Understanding the Risks of Taking Daily Aspirin
Aspirin is an over-the-counter drug, which can give a false sense of security. It is a powerful medication with significant potential side effects. For any medication to be worthwhile, its benefits must clearly outweigh its risks. Since the benefit of taking aspirin for high blood pressure is nonexistent, the decision to take it means you are accepting all the risk for no reward.
Why Aspirin is Not a “Vitamin for the Heart”
The widespread belief that daily aspirin is a harmless preventive measure is one of the most dangerous medical myths. The risks of taking daily aspirin are real and can be life-threatening.
The Major Risks
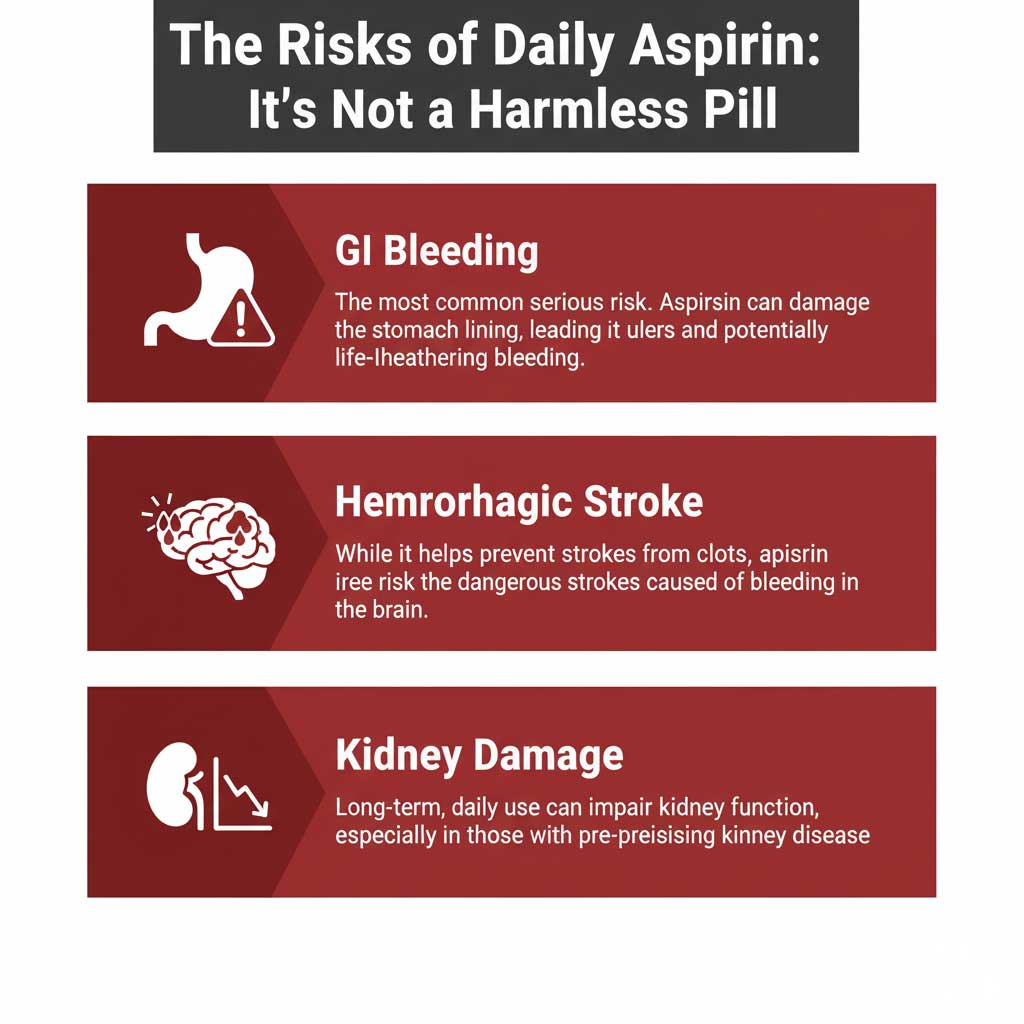
Aspirin Gastrointestinal Bleeding
This is the most common and well-known serious side effect. Aspirin works by blocking enzymes that protect the stomach lining. This can lead to irritation, ulcers, and serious gastrointestinal bleeding. The risk is higher in older adults and those with a history of ulcers.
Hemorrhagic Stroke (Brain Bleed)
This is a critical paradox of aspirin therapy. While it is effective at preventing strokes caused by blood clots (ischemic strokes), it simultaneously increases the risk of strokes caused by bleeding in the brain (hemorrhagic strokes).
Kidney Problems
Long-term, regular use of aspirin and other NSAIDs can impair kidney function and is generally discouraged for individuals with chronic kidney disease.
Interactions with Aspirin and Blood Pressure Medication
It is vital that your doctor knows you are taking daily aspirin, as it can interact with some of the medications prescribed to treat your high blood pressure. For example, some studies have suggested that high doses of aspirin might slightly reduce the effectiveness of common blood pressure drugs like ACE inhibitors, while taking it with diuretics could increase the risk of kidney issues.
Conclusion: The Final Verdict on Aspirin and Blood Pressure
So, after reviewing the highest quality scientific evidence, does aspirin lower blood pressure? The final verdict from the scientific and medical community is a clear no. Aspirin does not meaningfully lower blood pressure and should not be used as a treatment for hypertension. The small, inconsistent effects seen in some older, smaller studies have been largely disproven by larger, more reliable clinical trials.
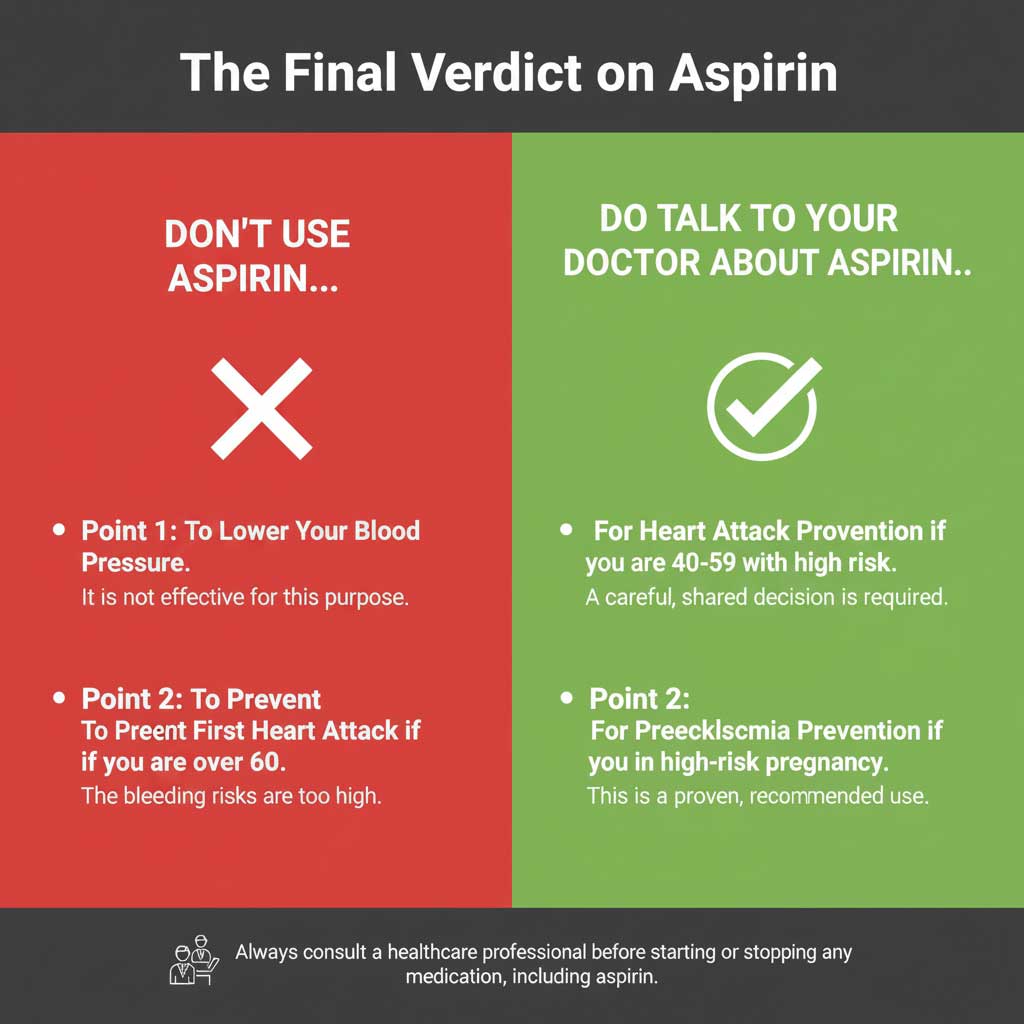
The evidence points to only two primary, evidence-backed uses for a daily low-dose aspirin:
- For the prevention of a first heart attack or stroke (primary prevention) in a very select group of adults aged 40-59 with high cardiovascular risk and low bleeding risk.
- For the prevention of preeclampsia in pregnant women who are identified as being at high risk.
The most important takeaway is that aspirin is a powerful medication with significant risks. You should never start or stop taking daily aspirin without first having a detailed conversation with your doctor. The decision must be a personal one, based on your unique health profile and a careful weighing of the potential benefits against the very real risks.
Frequently Asked Questions (FAQs)
1. So, should I stop taking my daily aspirin if I have high blood pressure?
You should never stop taking aspirin without talking to your doctor first. If you have a history of a heart attack, stroke, or have a stent, you are likely taking aspirin for “secondary prevention,” where the benefits are well-established and far outweigh the risks. Your high blood pressure is a separate issue that needs to be treated with appropriate medications.
2. I’m over 60. Do the new USPSTF guidelines mean I should stop my daily aspirin?
The new guidelines recommend against starting aspirin for primary prevention in adults 60 or older. They do not give a blanket recommendation for people in this age group who are already taking it to stop. This is a decision that must be individualized in a conversation with your healthcare provider, who can weigh your specific risks and benefits.
3. What’s the difference between the 81 mg “baby aspirin” and a regular 325 mg aspirin?
The 81 mg dose, often called “low-dose” or “baby aspirin,” is the standard dose used for long-term cardiovascular prevention. The 325 mg dose is a “regular strength” dose more commonly used for pain and fever relief. The anti-clotting benefits are present even at the low dose, with a slightly lower risk of bleeding.
4. Can taking aspirin give me a false reading on my home blood pressure monitor?
No. Aspirin does not have an acute or immediate effect on blood pressure and will not interfere with the accuracy of your home blood pressure monitor.
5. If aspirin doesn’t lower blood pressure, what are the best ways to do it?
The best, evidence-based ways to lower blood pressure include lifestyle changes (like a low-sodium diet, regular exercise, limiting alcohol, and managing stress) and taking antihypertensive medications as prescribed by your doctor.
6. I have a high cardiovascular risk. How do I know if my bleeding risk is also high?
Your doctor determines your bleeding risk by looking at factors such as your age, a history of stomach ulcers or GI bleeding, chronic kidney disease, a low platelet count, and your use of other medications that can increase bleeding, like other NSAIDs (ibuprofen, naproxen) or anticoagulant drugs.
7. Does taking aspirin affect my cholesterol levels?
No. Aspirin does not have any direct effect on your cholesterol levels (LDL, HDL, or triglycerides). Cholesterol is managed through diet, exercise, and medications like statins.
8. Why did doctors used to recommend aspirin so much more often?
Earlier research highlighted the benefits of aspirin more than the risks. Over the past decade, several large, high-quality clinical trials have given us a much clearer picture of the bleeding risks associated with aspirin, particularly in people who have not yet had a heart attack or stroke. This new data has led to the more cautious, restrictive guidelines we have today.
9. Can I take ibuprofen or other NSAIDs instead of aspirin for heart health?
No. In fact, you should be very careful. Other NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve) do not have the same anti-clotting properties as aspirin. Furthermore, they can actually increase blood pressure and the risk of heart attack and stroke, and can interfere with the cardiovascular benefits of aspirin if taken at the same time.
10. How long does it take for aspirin’s anti-clotting effect to start working?
The effect of aspirin on platelets is very rapid. When you take a dose of aspirin, it starts to inhibit platelet function within about an hour, and its effect on those platelets is permanent for their entire lifespan (about 7-10 days).

