You log into your patient portal to check your latest lab results. You scroll past the cholesterol and glucose numbers until you reach the Complete Blood Count (CBC). There are several lines of data, but one specific metric has been circled by your doctor or flagged in red. It is the absolute neutrophil count.
Table of Contents
For the average person, this number is just another medical statistic. However, for patients navigating chemotherapy, autoimmune disorders, or unexplained infections, the absolute neutrophil count (ANC) is the single most critical indicator of safety. It acts as the gatekeeper that determines whether your body is capable of defending itself against the invisible world of bacteria and fungi.
Understanding this number removes the fear of the unknown. It transforms a confusing medical report into a tool for empowerment. By mastering the meaning of your ANC, you can make informed decisions about your treatment schedule, your diet, and your daily interactions.
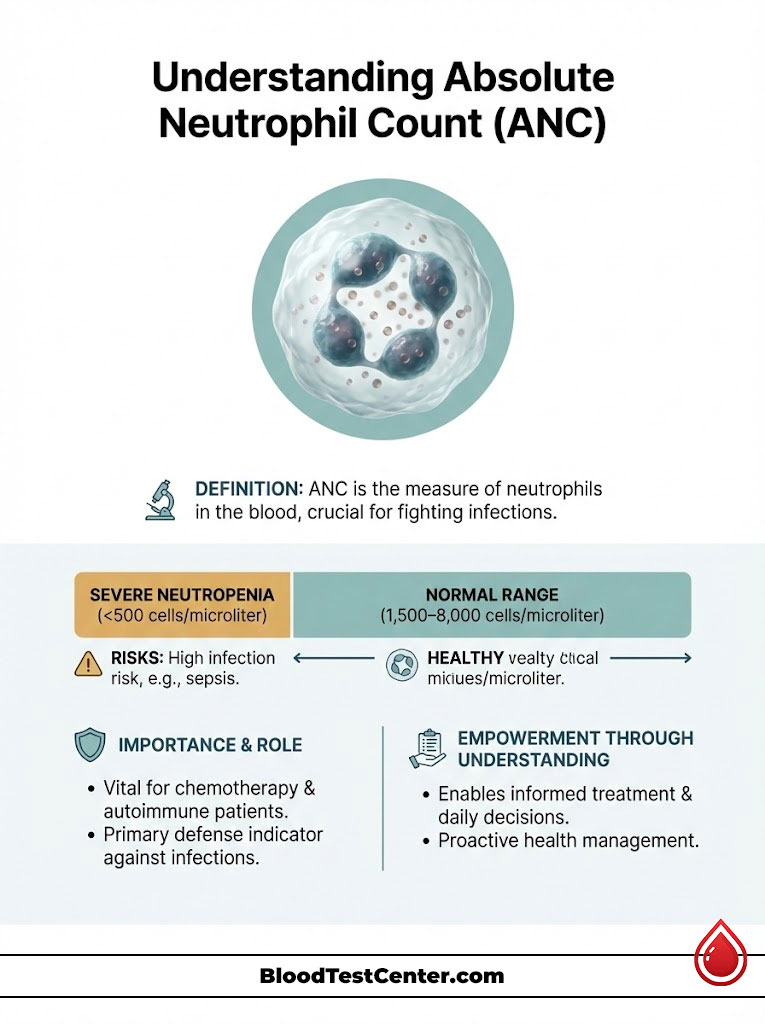
The Absolute Neutrophil Count (ANC) is a clinical calculation that measures the precise number of neutrophil granulocytes in a specific volume of blood. While the total white blood cell count provides a general overview of immune health, the ANC offers a targeted assessment of the body’s ability to fight bacterial infections. A normal ANC range typically falls between 1,500 and 8,000 cells per microliter of blood. Levels falling below 500 cells per microliter indicate severe neutropenia, a condition that requires immediate medical precautions due to the high risk of life-threatening sepsis.
Understanding the Absolute Neutrophil Count and Immune System Function
To truly grasp why the absolute neutrophil count matters, we must first understand the biology of the soldier it counts: the neutrophil. The human immune system is a complex network of defenses, but the neutrophil is the brute force of that army.
The Role of Neutrophils as First Responders
Neutrophils are the most abundant type of white blood cell in the human body. In a healthy adult, they comprise approximately 55% to 70% of the total leukocyte population. These cells are produced in the bone marrow, the spongy tissue inside your large bones.
When a pathogen such as a bacteria or fungus breaches the body’s barriers, neutrophils are the first responders. They engage in a biological process known as chemotaxis. This means they sense the chemical signals released by the invading bacteria and rapidly migrate toward the infection site. Once they arrive, they perform phagocytosis. They literally engulf and digest the enemy pathogens.
Without a sufficient number of these cells, the body loses its primary defense mechanism. This state of vulnerability is what makes the ANC blood test so vital. It is not just counting cells; it is measuring your biological armor.
Distinguishing Between Total WBC and Absolute Neutrophil Count
A frequent source of confusion for patients is the difference between the total White Blood Cell count (WBC) and the ANC. It is possible for a patient to have a normal total WBC count while simultaneously having a dangerously low absolute neutrophil count.
This discrepancy occurs because the total WBC count includes all five types of white blood cells: neutrophils, lymphocytes, monocytes, eosinophils, and basophils. If a patient has a viral infection, their lymphocytes might be elevated, artificially inflating the total WBC number. Meanwhile, their neutrophils could be critically depleted.
Oncologists and hematologists in the USA prioritize the ANC over the total WBC because bacterial infections are the most immediate threat to immunocompromised patients. The ANC cuts through the noise of the other cell types to provide a clear picture of bacterial defense.
Mastering the ANC Calculation Formula and Interpreting Blood Test Results
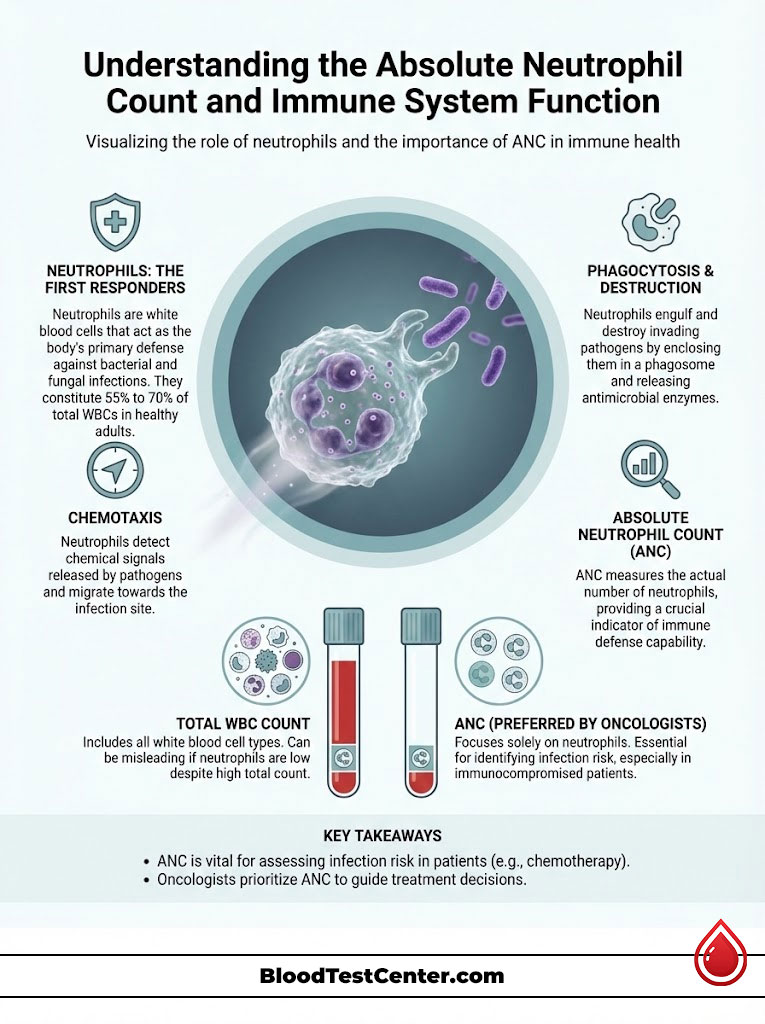
Your lab report might not always explicitly list the absolute neutrophil count. In many cases, the laboratory provides the components, and the medical team or the patient must perform the ANC calculation. Understanding how this number is derived demystifies the data.
Analyzing the Components: Segs and Bands
To calculate the ANC, you must look at the “differential” section of the CBC with differential. This section breaks down the white blood cells into their specific subtypes. You will see two terms that are essential for the formula:
- Segs (Segmented Neutrophils): These are the mature, fully functional workers. They have a segmented nucleus and are ready to fight infection immediately upon release from the marrow.
- Bands: These are immature neutrophils. They are the “reserves” that the bone marrow releases early when the body is under extreme stress or fighting an active infection.
When a doctor refers to a “left shift” in your blood work, they are noting an increase in bands. This indicates that your marrow is working overtime to pump out cells, suggesting an active battle against infection.
The Standard ANC Calculation Formula
The formula used by major diagnostic laboratories like LabCorp, Quest Diagnostics, and hospital systems across the USA is standardized.
The Formula:
ANC = Total WBC x [(% Segs + % Bands) / 100]
Real-World Instance of ANC Calculation
Let us examine a hypothetical patient scenario to see this math in action.
- Total WBC: 3,500 cells/µL (This is slightly low)
- Segs: 40%
- Bands: 5%
Step 1: Add the percentages of the neutrophils together.
40% (Segs) + 5% (Bands) = 45%.
Step 2: Convert the percentage to a decimal.
45% becomes 0.45.
Step 3: Multiply the total WBC by this decimal.
3,500 x 0.45 = 1,575.
In this instance, the patient’s absolute neutrophil count is 1,575 cells/µL. despite the low total WBC, their neutrophil count is technically within the safe range (above 1,500), allowing them to potentially proceed with treatment.
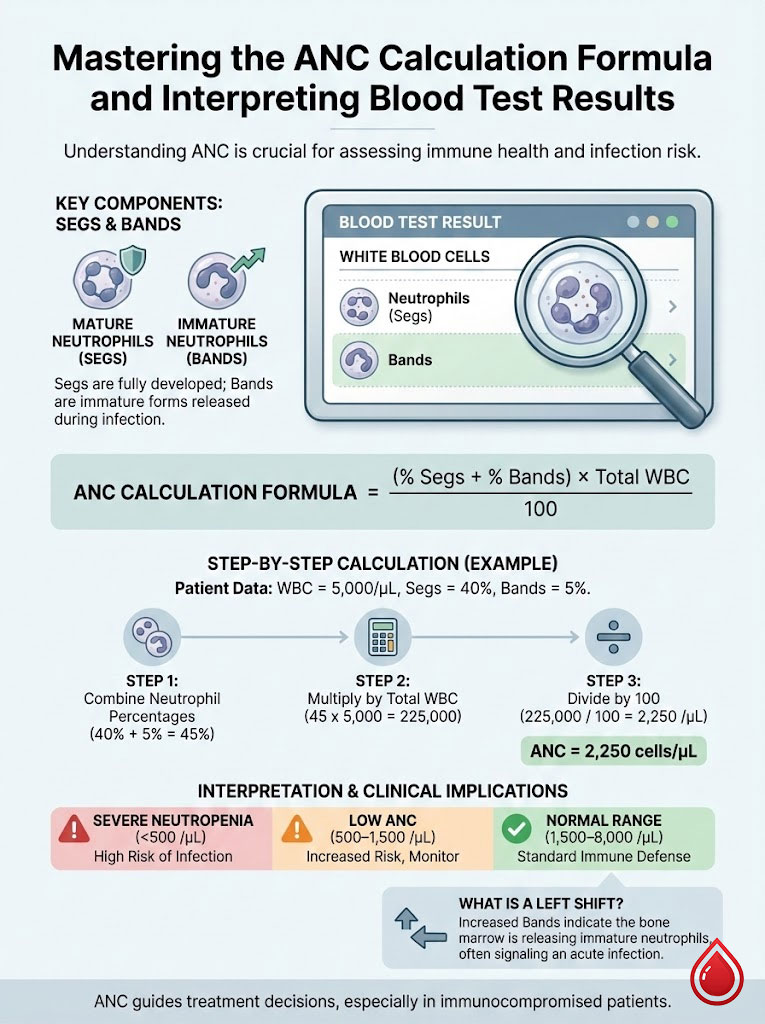
Decoding Normal ANC Ranges and Identifying Neutropenia Severity Levels
Once you have your number, the next step is interpretation. Clinical decisions are based on where your absolute neutrophil count falls within established risk categories.
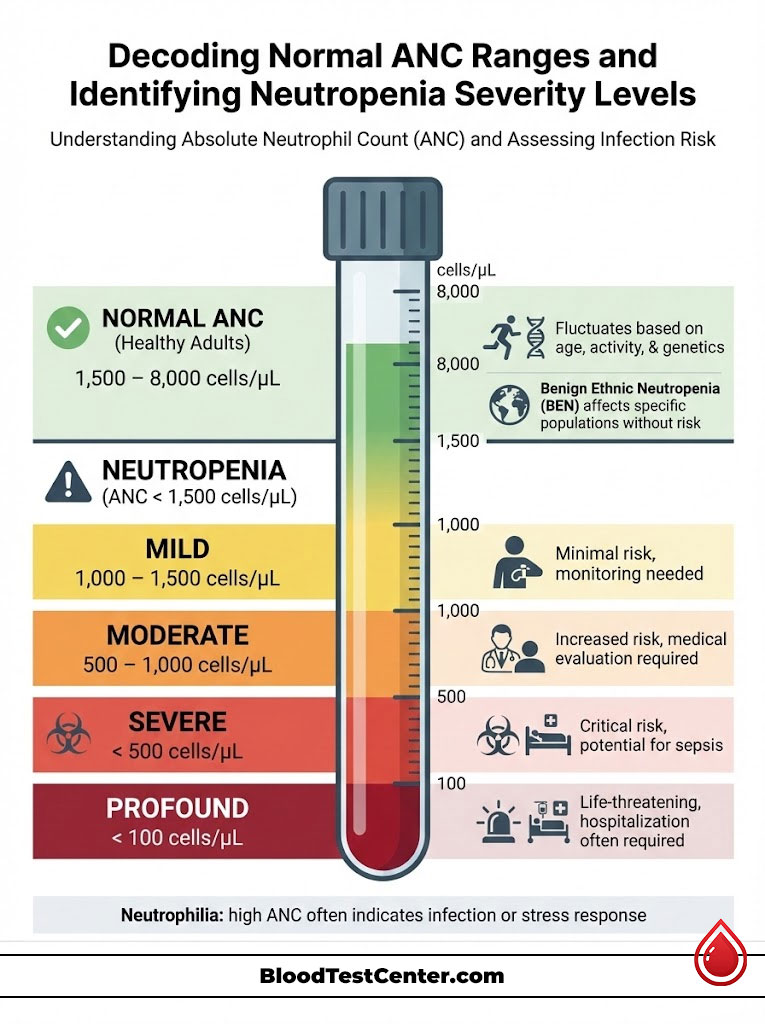
Defining the Normal ANC Range
For a healthy adult, a normal ANC range is widely accepted to be between 1,500 and 8,000 cells per microliter (cells/µL).
However, “normal” is not a static number. It can fluctuate based on age, activity level, and time of day. For example, infants and toddlers typically have different reference ranges than adults. Additionally, genetic factors play a significant role.
Benign Ethnic Neutropenia (BEN) is a recognized clinical entity. It is frequently observed in individuals of African, Middle Eastern, and West Indian descent. These individuals may consistently have an ANC between 1,000 and 1,500 without any increased risk of infection or health issues. It is vital for physicians to recognize this to avoid unnecessary testing or treatment delays.
The Danger Zones: Categorizing Neutropenia Severity
When the ANC drops below 1,500, the condition is medically termed neutropenia. The severity of neutropenia dictates the medical response. The lower the number drops, the higher the probability of a severe infection.
| Severity Level | ANC Range (cells/µL) | Clinical Risk and Medical Action |
| Normal Range | 1,500 – 8,000 | The immune system is fully operational. The body can fight off standard environmental pathogens without assistance. |
| Mild Neutropenia | 1,000 – 1,500 | There is a minimal infection risk. Most patients are asymptomatic. Doctors may monitor counts more frequently but rarely delay chemotherapy. |
| Moderate Neutropenia | 500 – 1,000 | The risk of infection increases. Any fever requires immediate medical evaluation. Chemotherapy doses may be reduced or delayed. |
| Severe Neutropenia | < 500 | Critical Risk Zone. The body has virtually no defense against endogenous bacteria (bacteria already inside the gut or on the skin). High risk of sepsis. |
| Profound Neutropenia | < 100 | This is a life-threatening emergency state. Patients often require hospitalization, isolation, and prophylactic antibiotics. |
Understanding Neutrophilia (High ANC)
While low counts are the primary concern in oncology, a high absolute neutrophil count is called neutrophilia. This is typically a sign that the body is currently fighting a bacterial infection. The marrow is dumping cells into the bloodstream to aid the defense.
However, high counts can also be caused by non-infectious factors. Physical trauma, surgery, high-stress levels, and cigarette smoking can elevate the ANC. Furthermore, medications such as corticosteroids (like Prednisone) cause neutrophils to detach from blood vessel walls and enter the bloodstream, artificially spiking the count.
The Critical Role of Absolute Neutrophil Count During Chemotherapy and Cancer Treatment
For millions of patients in the USA undergoing cancer treatment, the absolute neutrophil count is the governing metric of their lives. It determines the rhythm of their therapy and the safety of their daily existence.
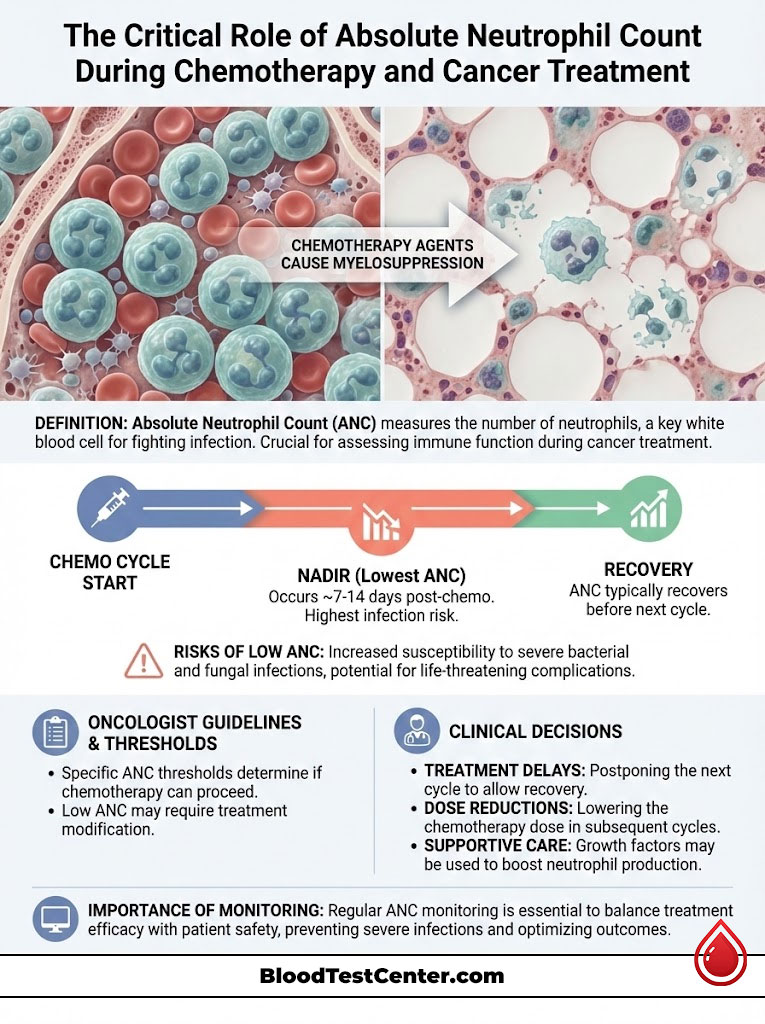
The Mechanism of Chemotherapy-Induced Neutropenia
Most traditional chemotherapy agents are cytotoxic. This means they are designed to kill rapidly dividing cells. Cancer cells are targeted because they divide uncontrollably. However, the cells in the bone marrow that produce neutrophils are also rapid dividers.
When chemotherapy drugs enter the system, they cannot distinguish between a tumor cell and a healthy bone marrow stem cell. As a result, the bone marrow is temporarily suppressed. This is known as myelosuppression. The production of new white blood cells slows down or stops completely.
The Concept of the Nadir
The drop in blood counts is not immediate. Because neutrophils live for a short time (often less than a day), the existing supply is used up quickly, and no new reinforcements are arriving.
This leads to a point called the nadir. The nadir is the lowest point that blood counts will reach during a treatment cycle. Typically, this occurs between 7 and 14 days after the chemotherapy infusion. This is the period of highest danger for the patient. After the nadir, the marrow usually begins to recover, and the absolute neutrophil count rises again in time for the next cycle.
Clinical Decisions: Delays and Dose Reductions
Oncologists follow strict safety protocols based on the ANC blood test. The standard threshold for administering a dose of chemotherapy is usually an ANC of 1,500 cells/µL.
If a patient arrives for their infusion and their ANC is 900, the treatment is typically cancelled. The patient is sent home to wait for their marrow to recover. These delays can be frustrating and anxiety-inducing, as patients worry about the cancer growing during the break. However, administering chemo to a patient with a low ANC could lead to fatal complications.
If delays happen frequently, the oncologist may reduce the dosage of the chemotherapy drug to spare the bone marrow, or they may introduce growth factors to support the counts.
Recognizing Non-Cancer Causes of Low Absolute Neutrophil Count
While cancer treatment is the most prominent cause of low ANC, it is not the only one. Patients with other medical histories may experience neutropenia due to different mechanisms.
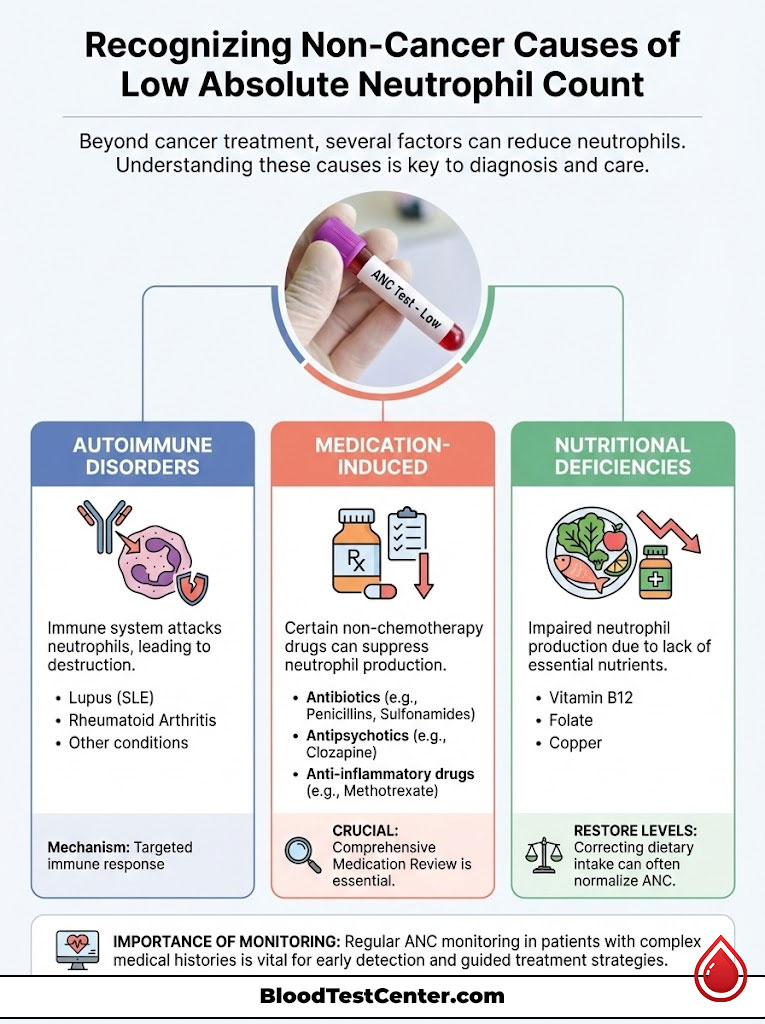
Autoimmune Disorders and Chronic Conditions
In certain autoimmune diseases, the body’s immune system becomes confused and begins to attack its own cells.
- Lupus (SLE): Patients with Lupus often have antibodies that target and destroy their own neutrophils, leading to chronic neutropenia.
- Rheumatoid Arthritis: A rare complication known as Felty’s Syndrome involves the triad of rheumatoid arthritis, an enlarged spleen, and a dangerously low absolute neutrophil count.
Medication-Induced Neutropenia
Pharmacists and doctors must always review a patient’s medication list when ANC drops unexpectedly. Several non-chemo drugs are known offenders:
- Antibiotics: Long-term use of strong antibiotics like Vancomycin or Penicillin G can suppress marrow.
- Psychotropic Drugs: Clozapine, an antipsychotic medication, carries a specific warning for causing agranulocytosis (a complete lack of granulocytes). Patients on this drug require regular ANC blood tests mandated by a federal registry.
- Antithyroid Medications: Drugs like Methimazole, used for Graves’ disease, can occasionally cause a sudden drop in counts.
Nutritional Deficiencies
The production of neutrophils is a resource-intensive process. The bone marrow requires specific micronutrients to build DNA and cellular structures. Severe deficiencies in Vitamin B12, Folate (Vitamin B9), or Copper can lead to ineffective hematopoiesis. In these cases, correcting the diet or supplementing the vitamin often restores the normal ANC range.
Proven Strategies for Managing Low Absolute Neutrophil Count and Preventing Infection
When the absolute neutrophil count is low, the patient is living in a “defensive mode.” There are two main approaches to management: medical intervention to raise the count and lifestyle changes to avoid infection.

Medical Interventions: G-CSF Injections
In modern oncology, doctors have a powerful tool to prevent prolonged neutropenia. These are called Granulocyte Colony-Stimulating Factors (G-CSF).
Common brand names include Neupogen (Filgrastim), Neulasta (Pegfilgrastim), and biosimilars like Zarxio. These are synthetic versions of a hormone the body naturally produces. When injected, usually 24 hours after chemotherapy, they travel to the bone marrow and violently stimulate the stem cells to produce neutrophils.
These drugs can significantly shorten the duration of the nadir and reduce the risk of hospitalization. However, they come with side effects, most notably deep bone pain as the marrow expands rapidly inside the bones.
The Neutropenic Diet and Food Safety
For decades, patients with low ANC were placed on a strict “Neutropenic Diet.” This diet forbade all fresh fruits and vegetables. Recent research has led to a relaxation of these rules in many USA cancer centers, shifting the focus from avoidance to rigorous safety and hygiene.
The goal is to eliminate bacterial load from food sources.
| Food Category | Safe (Eat This) | Unsafe (Avoid This) |
| Dairy Products | Pasteurized milk, yogurt, and commercial hard cheeses (Cheddar, Swiss). | Unpasteurized (raw) milk, soft cheeses with mold (Brie, Camembert, Blue Cheese), yogurt from soft-serve machines. |
| Fruits & Vegetables | Cooked vegetables, canned fruits, thick-skinned fruits (bananas, oranges, melons) that are washed and peeled. | Raw vegetable sprouts (alfalfa, bean), unwashed leafy greens, berries (difficult to clean thoroughly), fresh salsas. |
| Proteins | Well-cooked meat (no pink), hard-boiled eggs, canned tuna/chicken. | Sushi, sashimi, rare or medium-rare steak, runny eggs (over easy), raw oysters or clams. |
| Beverages | Bottled water, boiled tap water, canned soda, pasteurized juices. | Well water (unless tested recently), unsterilized spring water, cold-brewed tea made with sun. |
| Deli & Fast Food | Freshly cooked hot meals. | Cold cuts from deli counters, salad bars, buffets where food sits out. |
Lifestyle and Environmental Precautions
Beyond diet, patients must modify their environment to reduce exposure to pathogens.
- Hand Hygiene: This is the single most effective prevention strategy. Frequent washing with soap and water for 20 seconds is non-negotiable.
- Gardening: Soil is rich in bacteria and fungal spores (like Aspergillus). Patients with low ANC should avoid gardening, mulching, or repotting plants.
- Pet Safety: While pets provide comfort, they also carry risks. Patients should not change cat litter boxes (toxoplasmosis risk) or handle dog waste. Being licked on the face by a pet should be avoided due to oral bacteria.
- Dental Care: The mouth is a primary entry point for bacteria. Chemotherapy can cause mucositis (mouth sores). Using a soft-bristled toothbrush and avoiding alcohol-based mouthwashes helps maintain the mucosal barrier.
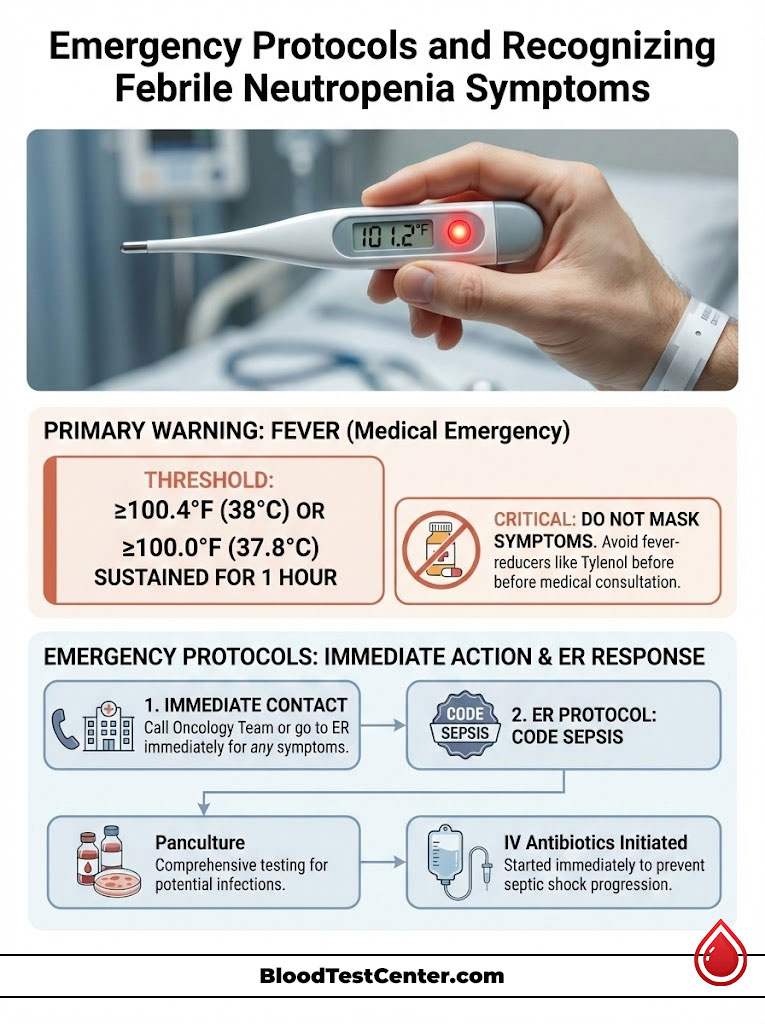
Emergency Protocols and Recognizing Febrile Neutropenia Symptoms
Despite the best precautions, infections can occur. For a patient with a low absolute neutrophil count, time is the enemy. The body cannot mount an inflammatory response, so the usual signs of infection (swelling, pus, redness) may be absent.
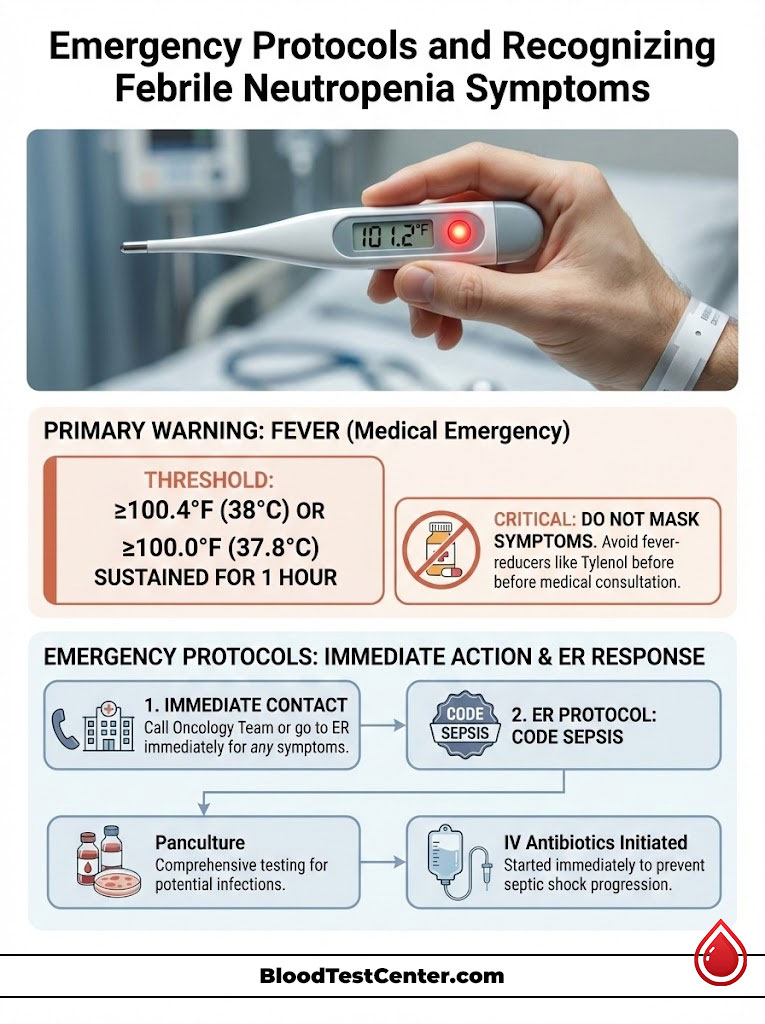
The Significance of Fever
The only warning sign might be a fever. In the context of low ANC, a fever is not just a symptom; it is a medical emergency known as febrile neutropenia.
The clinical threshold is a single oral temperature of 100.4°F (38°C) or higher, or a temperature of 100.0°F (37.8°C) sustained for one hour.
Patients are often advised not to take fever-reducing medications like Tylenol (Acetaminophen) because these drugs can mask the fever, delaying the diagnosis of a potentially fatal infection.
The “Call the Doctor” Checklist
Patients and caregivers should immediately contact their oncology team or go to the Emergency Room if they experience:
- Fever over 100.4°F.
- Chills or rigors (uncontrollable shaking).
- Shortness of breath or rapid heartbeat.
- Confusion or dizziness.
- Pain or redness around a central line (Port or PICC line).
ER Procedures for Neutropenic Patients
When a neutropenic patient arrives at the ER, it is treated as a “Code Sepsis.” The medical team will immediately perform a “panculture.” This involves drawing blood from peripheral veins and the central line, collecting urine samples, and sometimes performing a chest X-ray.
Crucially, IV antibiotics are usually started immediately, often before the source of infection is even identified. This preemptive strike is necessary because, without neutrophils, a bacterial infection can progress to septic shock in a matter of hours.
Summary & Key Takeaways
Navigating a diagnosis that involves monitoring blood counts can be overwhelming, but knowledge is your best defense. The absolute neutrophil count is the true measure of your safety during treatment, far more specific and actionable than the general white blood cell count.
- The Critical Number: An ANC below 500 cells/µL places you in the danger zone for severe infection.
- The Calculation: Remember that ANC is derived from the sum of your mature cells (Segs) and your immature reserves (Bands).
- The Nadir: Expect your counts to be at their lowest 7 to 14 days after a chemotherapy cycle; this is the time for maximum vigilance.
- The Action Plan: Prioritize food safety by following the neutropenic diet, practice rigorous hand hygiene, and treat any fever of 100.4°F as an immediate emergency.
By partnering with your medical team and monitoring your ANC blood test results, you can actively participate in your care, ensuring that you remain safe while your body fights for recovery.
Frequently Asked Questions (FAQ)
What is considered a critically low absolute neutrophil count?
A count below 500 cells per microliter is clinically defined as severe neutropenia. At this level, the risk of developing a serious bacterial infection increases exponentially because the body lacks the soldiers to fight off even normal flora from the gut or skin.
How can I raise my absolute neutrophil count fast?
The only scientifically proven method to rapidly increase ANC is through the use of Granulocyte Colony-Stimulating Factor (G-CSF) injections, such as Neulasta or Neupogen. These drugs stimulate the bone marrow to release neutrophils within 24 to 48 hours. No specific food or vitamin supplement works instantly.
Does absolute neutrophil count fluctuate daily?
Yes, the ANC is a dynamic number. Neutrophils have a very short lifespan, often living only 6 to 12 hours in the bloodstream. Consequently, counts can fluctuate based on the time of day, physical activity levels, and physiological stress.
Can anxiety cause low absolute neutrophil count?
While chronic stress can negatively impact the immune system over time, anxiety itself is not a direct cause of clinical neutropenia. Conversely, acute stress or panic attacks can sometimes cause a temporary spike in the count (neutrophilia) due to the release of adrenaline.
What is the difference between neutrophils and absolute neutrophil count?
“Neutrophils” are the physical cells circulating in your blood. The “Absolute Neutrophil Count” is the mathematical measurement of those cells. Think of neutrophils as the cars and the ANC as the traffic count report; one is the object, the other is the data point.
Is an ANC of 1,500 safe for chemotherapy?
Yes, an ANC of 1,500 cells/µL is the standard safety benchmark used by most oncologists in the USA. If a patient meets this threshold, they are generally cleared to receive their next dose of chemotherapy.
What does a high absolute neutrophil count mean?
A high ANC (Neutrophilia) usually indicates that the body is actively fighting a bacterial infection. It can also be a side effect of steroid medications like Prednisone, or a result of significant physical trauma, surgery, or burns.
Can I eat salad with low ANC?
If you have severe neutropenia (<500), most medical guidelines advise against eating raw salads. Leafy greens have a high surface area that can harbor bacteria like E. coli and Salmonella, which are difficult to wash off completely. Cooked vegetables are a safer alternative.
What is Benign Ethnic Neutropenia?
Benign Ethnic Neutropenia is a genetic trait commonly found in people of African, Middle Eastern, and West Indian heritage. These individuals have a naturally lower normal ANC range but have fully functional immune systems and do not suffer from increased infection rates.
How do I calculate ANC from percentages?
To calculate ANC manually, multiply your total white blood cell count by the decimal sum of your segmented neutrophils and bands. For example: Total WBC 4,000 x (0.40 Segs + 0.10 Bands) = 2,000 ANC.
Why are “bands” important in ANC?
Bands are immature neutrophils that have not yet fully developed their segmented nucleus. A high number of bands, known as a “left shift,” serves as an early warning system that the bone marrow is responding to a significant infection or stressor.
How long after chemo does ANC drop?
The ANC typically begins to decline about one week after a chemotherapy infusion. It reaches the nadir (lowest point) between days 7 and 14. Recovery usually begins shortly after, allowing counts to return to baseline by day 21 for the next cycle.
Disclaimer: The content provided in this article is for educational and informational purposes only. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or blood test results. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
References:
- American Cancer Society. "Understanding Your Lab Test Results."
- Mayo Clinic. "Neutropenia (low neutrophil count)."
- Centers for Disease Control and Prevention (CDC). "Preventing Infections in Cancer Patients."
- National Comprehensive Cancer Network (NCCN). "Guidelines for Management of Neutropenia."
- Leukemia & Lymphoma Society. "Blood Tests and Counts."