You get a blood pressure reading at a pharmacy kiosk or during a routine check-up, and the numbers are surprisingly high. You start to worry, running through the usual suspects—too much salt, not enough exercise, maybe stress? But what if the answer is far simpler and hiding in plain sight? Could that high reading be connected to the amount of water you drank—or didn’t drink—that day?
Table of Contents
The question is a critical one: Does dehydration cause high blood pressure? The answer, backed by a growing body of medical research, is a surprising and resounding yes. The intricate relationship between your hydration and blood pressure is one of the most overlooked, yet most fundamental, aspects of cardiovascular health.
This comprehensive guide from BloodTestCenter.com will explore this connection in detail. From a biological standpoint, dehydration triggers a powerful, ancient survival response that is specifically designed to increase your blood pressure. Understanding this mechanism is the first step toward using proper hydration as a simple, free, and incredibly effective tool for managing your blood pressure and overall health.
The Science of Scarcity: How Dehydration Raises Blood Pressure
To understand why a lack of water can make your blood pressure go up, you have to think like your body. Your body’s number one priority is survival, which means ensuring that your vital organs—your brain, heart, and kidneys—are constantly supplied with oxygen-rich blood. When you become dehydrated, your body initiates a brilliant, multi-step defense plan to make sure this happens, even with limited resources.
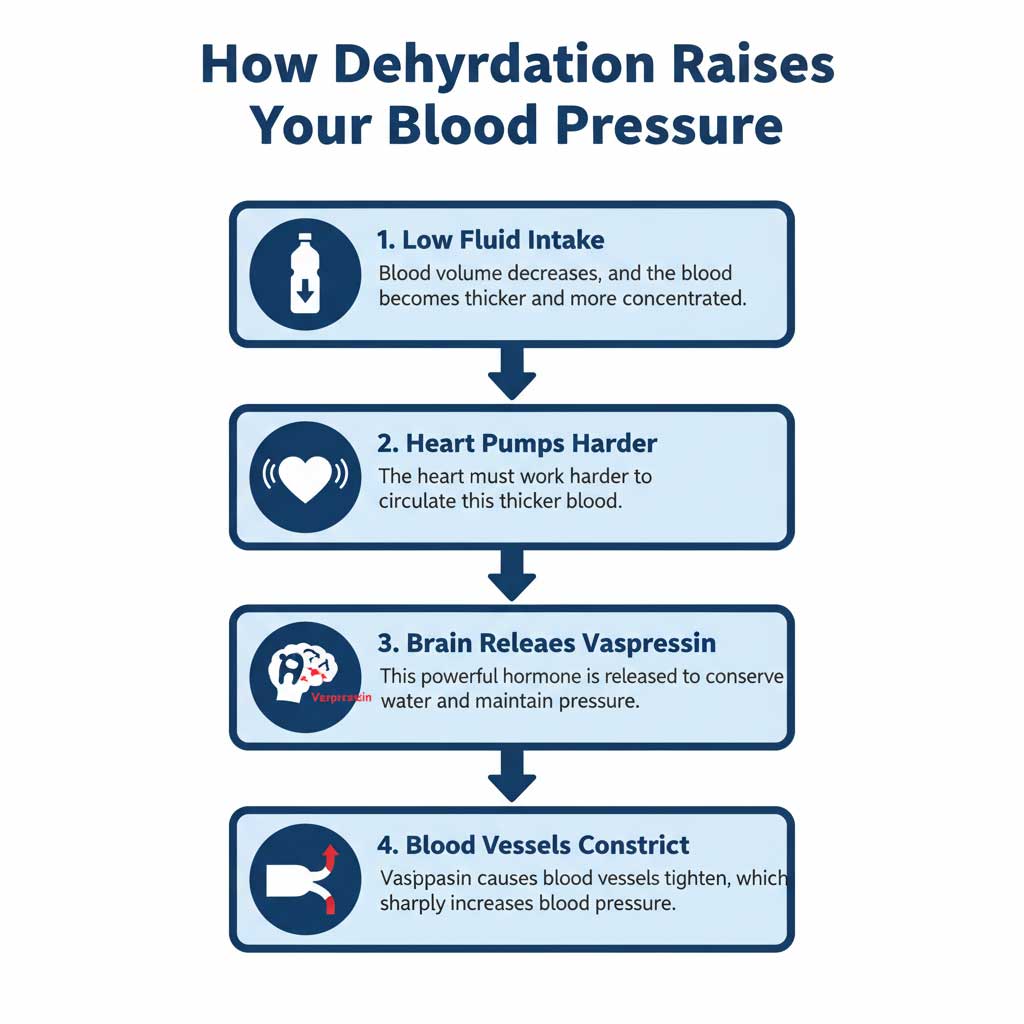
Step 1: Blood Volume Decreases
When you don’t drink enough fluid, the total volume of blood circulating through your arteries and veins begins to drop. Imagine a river during a drought: as the water level goes down, the remaining water becomes more concentrated and sludgy. The same thing happens in your bloodstream. The plasma (the liquid component of your blood) decreases, causing the blood to become thicker and more viscous.
Step 2: The Heart Works Harder
This thicker, more concentrated blood is significantly harder to move. In response, your heart muscle must pump with more force to push this sludgy blood through your circulatory system to reach all your tissues. This increased effort from your heart is the first factor that contributes to a higher blood pressure reading.
Step 3: The Hormonal Response – Vasopressin is Released
This is the scientific key to the entire process. Your brain, specifically the pituitary gland, is a master sensor. It constantly monitors your blood’s volume and its concentration of sodium. When it detects that your blood volume is low and your sodium level is high (a classic sign of dehydration), it releases a powerful hormone called vasopressin, also known as antidiuretic hormone (ADH).
Step 4: The Dual Action of Vasopressin
The relationship between vasopressin and blood pressure is direct and powerful. This hormone has two primary jobs, both of which are designed to conserve water and maintain pressure:
- Kidney Action: Vasopressin travels to your kidneys and gives them a direct order: “Stop making urine and reabsorb every last drop of water back into the body.” This is a crucial water-conservation step.
- Blood Vessel Action (Vasoconstriction): At the same time, vasopressin causes the smooth muscles that line your smaller blood vessels (your arterioles) to tighten and constrict. This makes the vessels narrower.
Think of it like putting your thumb over the end of a garden hose. The volume of water hasn’t changed, but by making the opening smaller, the pressure of the water shooting out increases dramatically. This vasoconstriction is a major reason dehydration and blood pressure are so closely linked.
The final result is a perfect storm for a high blood pressure reading: your heart is pumping harder to move thicker blood through pipes that have just been made narrower.
The Blood Pressure Paradox: Can Dehydration Also Cause LOW Blood Pressure?
One of the most common points of confusion is the question, “can dehydration raise or lower blood pressure?” You may have heard that someone who collapsed from heat stroke had dangerously low blood pressure. How can both be true? The answer lies in the severity and speed of the dehydration.
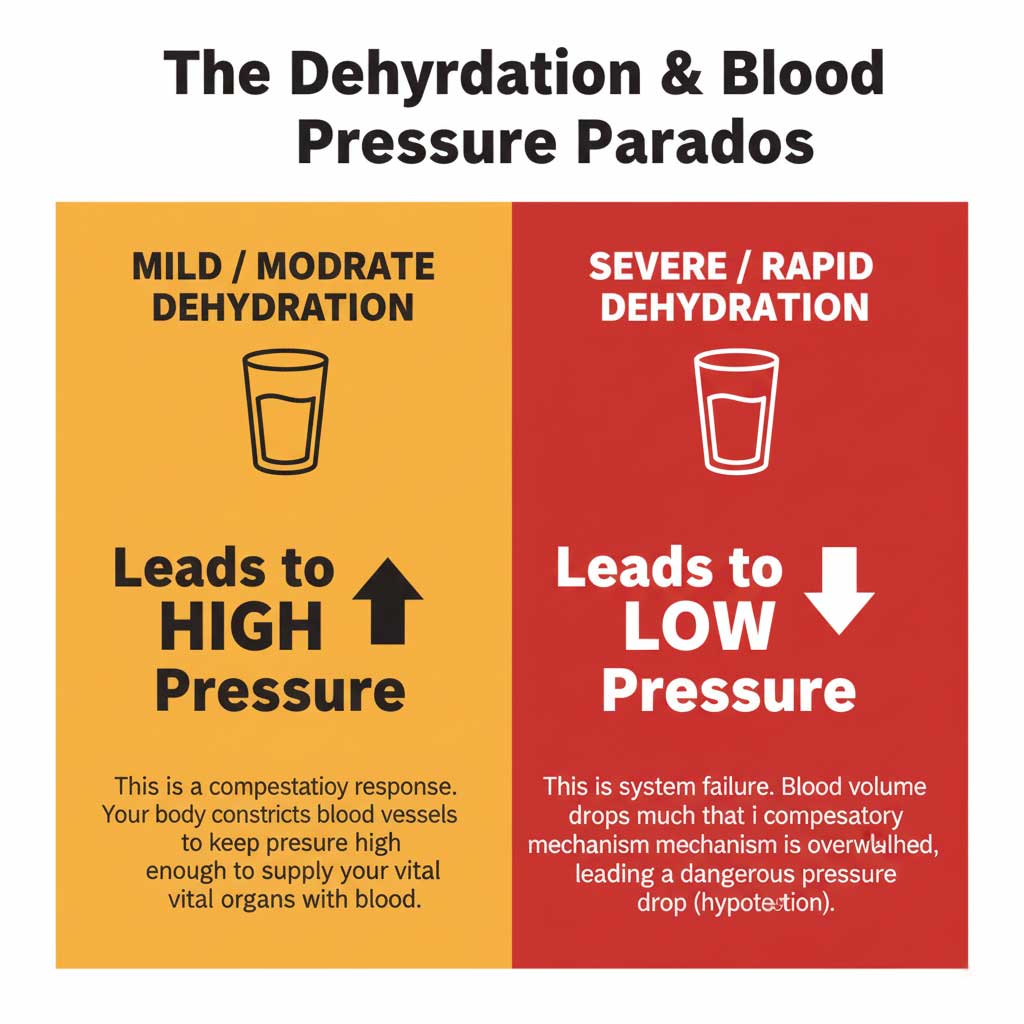
Mild to Moderate Dehydration -> HIGH Blood Pressure
In cases of everyday, mild dehydration high blood pressure is the body’s intelligent compensatory response. The release of vasopressin and the resulting vasoconstriction are your body’s way of artificially keeping the pressure high enough to ensure your brain and other organs get the oxygen they need, even with reduced blood volume. It’s a temporary fix and a clear sign that you need to drink water.
Severe and Rapid Dehydration -> LOW Blood Pressure (Hypotension)
In acute and severe situations—such as a person suffering from heat stroke, severe vomiting, or a traumatic injury—the body’s loss of fluid is so rapid and massive that the compensatory system is overwhelmed and fails. Blood volume plummets to a critical level, and there simply isn’t enough fluid left in the pipes to maintain any pressure at all. This leads to a dangerous drop in blood pressure, a condition known as dehydration and low blood pressure (hypotension), which can quickly lead to shock and organ failure.
Recognizing the Signs and Identifying High-Risk Groups
Because the body’s response to dehydration and blood pressure can be subtle, it’s important to know the signs and understand who is most at risk.
Common Symptoms of Dehydration
Often, the signs of dehydration high blood pressure are simply the classic symptoms of dehydration itself. These include:
- Thirst and a dry, sticky mouth
- Fatigue and a feeling of sluggishness
- Urinating less frequently, with urine that is dark yellow
- Headaches and dizziness
- In some cases, dehydration heart palpitations can occur as electrolyte imbalances (especially in sodium and potassium) disrupt the heart’s normal electrical rhythm.
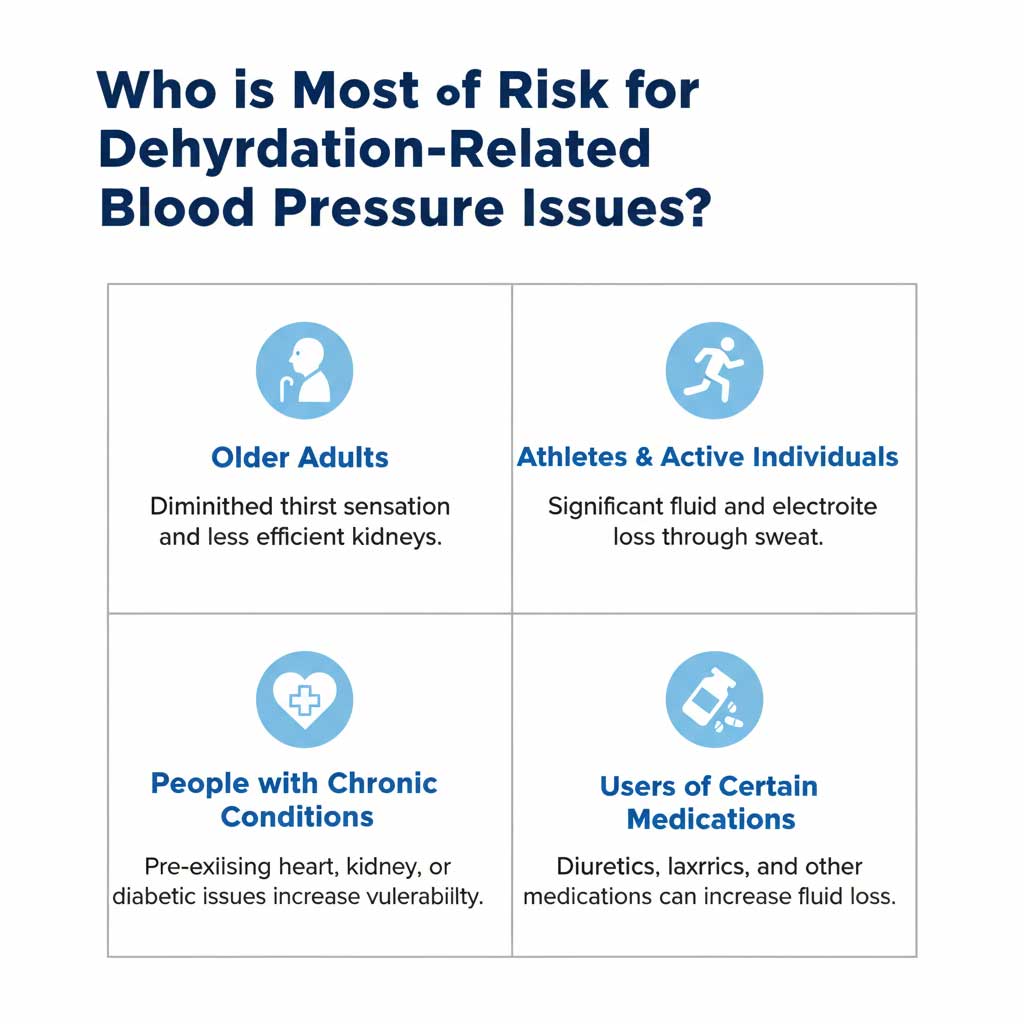
Who is Most at Risk?
While anyone can become dehydrated, certain groups are more vulnerable to its effects on blood pressure:
- Older Adults: The sense of thirst can diminish significantly with age, meaning seniors may not realize they are dehydrated until they are already experiencing symptoms. Their kidneys are also often less efficient at conserving water.
- Athletes and Outdoor Workers: People who sweat heavily, especially in hot U.S. states like Texas or Arizona, lose large amounts of both fluid and electrolytes. Without proper replacement, this can quickly trigger the vasopressin response.
- Individuals with Chronic Conditions: People with pre-existing heart disease, kidney problems, or diabetes are more susceptible to the cardiovascular strain caused by dehydration.
- People on Certain Medications: Diuretics, often called “water pills,” are commonly prescribed for high blood pressure. While effective, they increase fluid loss and can inadvertently raise the risk of dehydration if intake isn’t increased.
Hydration as a Tool: How to Drink for Better Blood Pressure
The good news is that understanding the link between hydration and blood pressure gives you a powerful and accessible tool for managing your health.
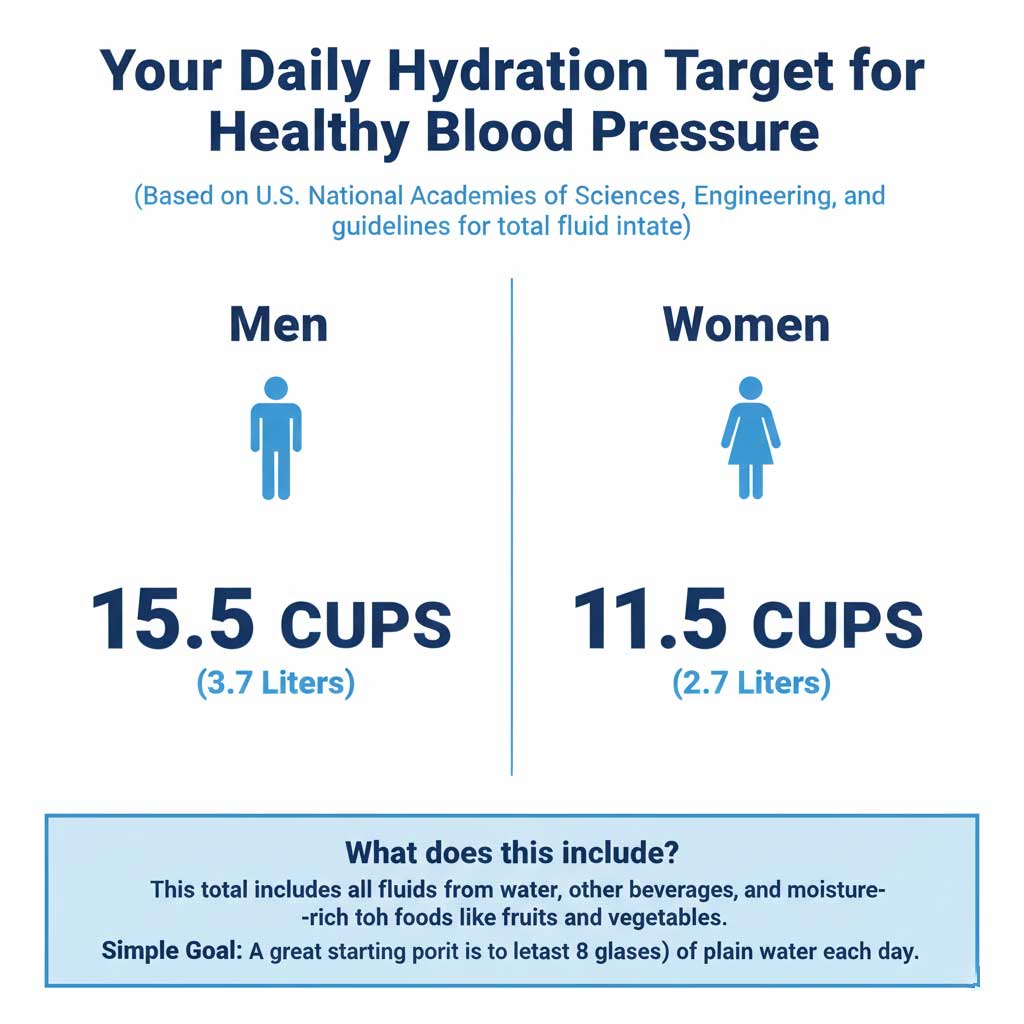
How Much Water Should I Drink Daily?
While the old “8 glasses a day” rule is a good starting point, official U.S. guidelines are more specific. The National Academies of Sciences, Engineering, and Medicine recommend a total daily fluid intake of:
- Approximately 15.5 cups (3.7 liters) for men
- Approximately 11.5 cups (2.7 liters) for women
This total includes fluids from all beverages and foods (about 20% of our daily fluid intake comes from moisture-rich foods like fruits and vegetables). The best gauge is the color of your urine—it should be consistently light yellow.
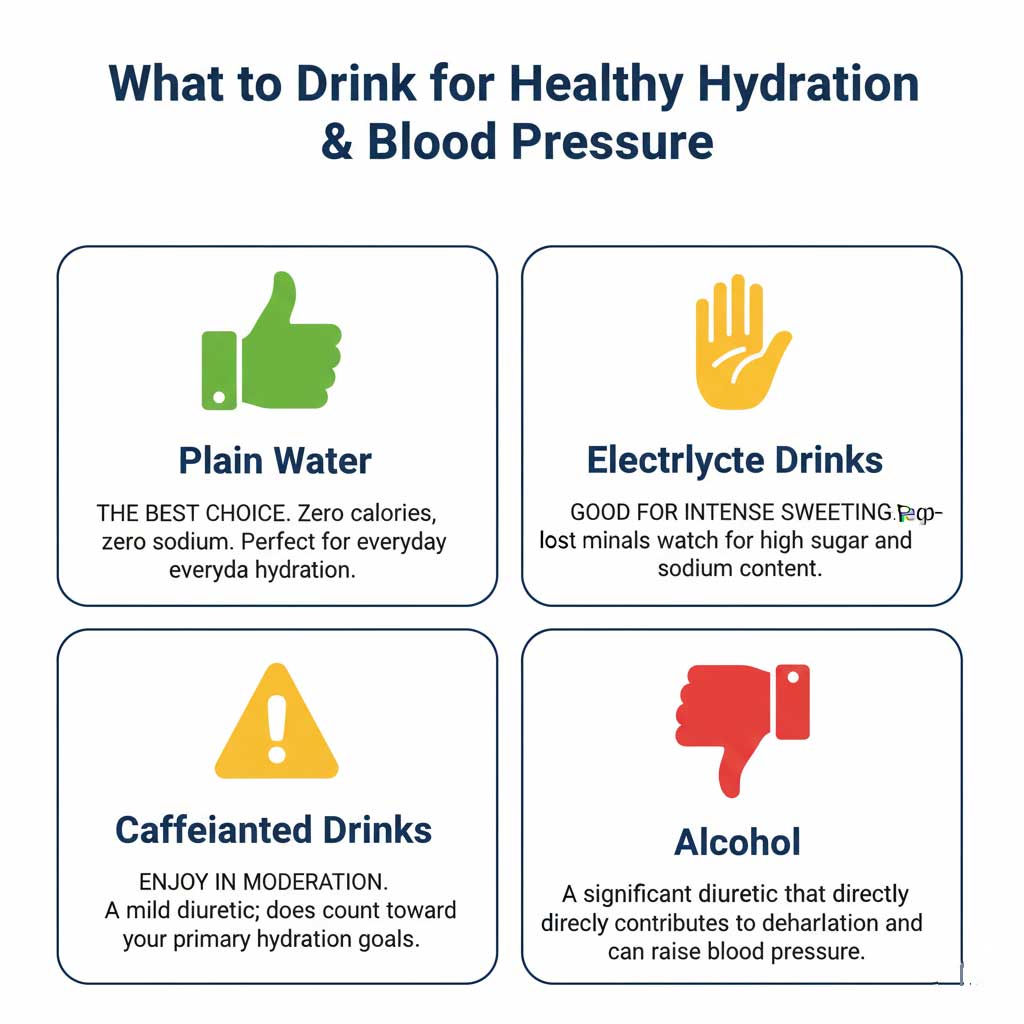
| Beverage Type | How it Affects Hydration & Blood Pressure | Best For… | U.S. Expert Guideline (e.g., from AHA) |
| Plain Water | The gold standard. Zero calories, zero sodium. Effectively restores blood volume and allows the body to regulate blood pressure naturally. | Everyday Hydration. The best choice for the vast majority of your daily fluid needs. | The American Heart Association recommends water as the best choice for a heart-healthy lifestyle to manage blood pressure. |
| Electrolyte Drinks | Replaces lost fluids plus key minerals like sodium and potassium lost through sweat. Can be beneficial for rehydration after intense activity. | Intense/Prolonged Exercise (>60 min). Also for heavy sweating in hot climates or during illness (vomiting/diarrhea). | Choose low-sugar options. If you have hypertension, be mindful of the sodium content and opt for low-sodium versions if possible. |
| Caffeinated Drinks (Coffee, Tea) | Mild diuretic effect, meaning it can cause you to lose more fluid through urine. This can contribute to dehydration if consumed in large quantities without other fluids. | Moderate Consumption. Enjoy in moderation, but do not count it as your primary source of hydration. | The U.S. Dietary Guidelines state that up to 400 mg of caffeine per day (about 4 cups of coffee) can be part of a healthy diet. |
| Alcoholic Drinks (Beer, Wine) | Significant diuretic effect. Alcohol suppresses the release of vasopressin, causing your kidneys to flush out more water than you consume. | Very Limited Consumption. Directly contributes to dehydration and can independently raise blood pressure. | The AHA recommends limiting alcohol to 2 drinks per day for men and 1 drink per day for women. |
How Long Does It Take to See a Change?
One of the most remarkable things about dehydration-related high blood pressure is how quickly it can respond to rehydration. If a high reading is primarily due to mild dehydration, your blood pressure can begin to normalize within 30 to 60 minutes of drinking one or two large glasses of water.
The Clinical Perspective: Diagnosis and Treatment
When a patient presents with a high blood pressure reading, a healthcare provider will often consider dehydration as a potential contributing factor, especially if other risk factors are present.
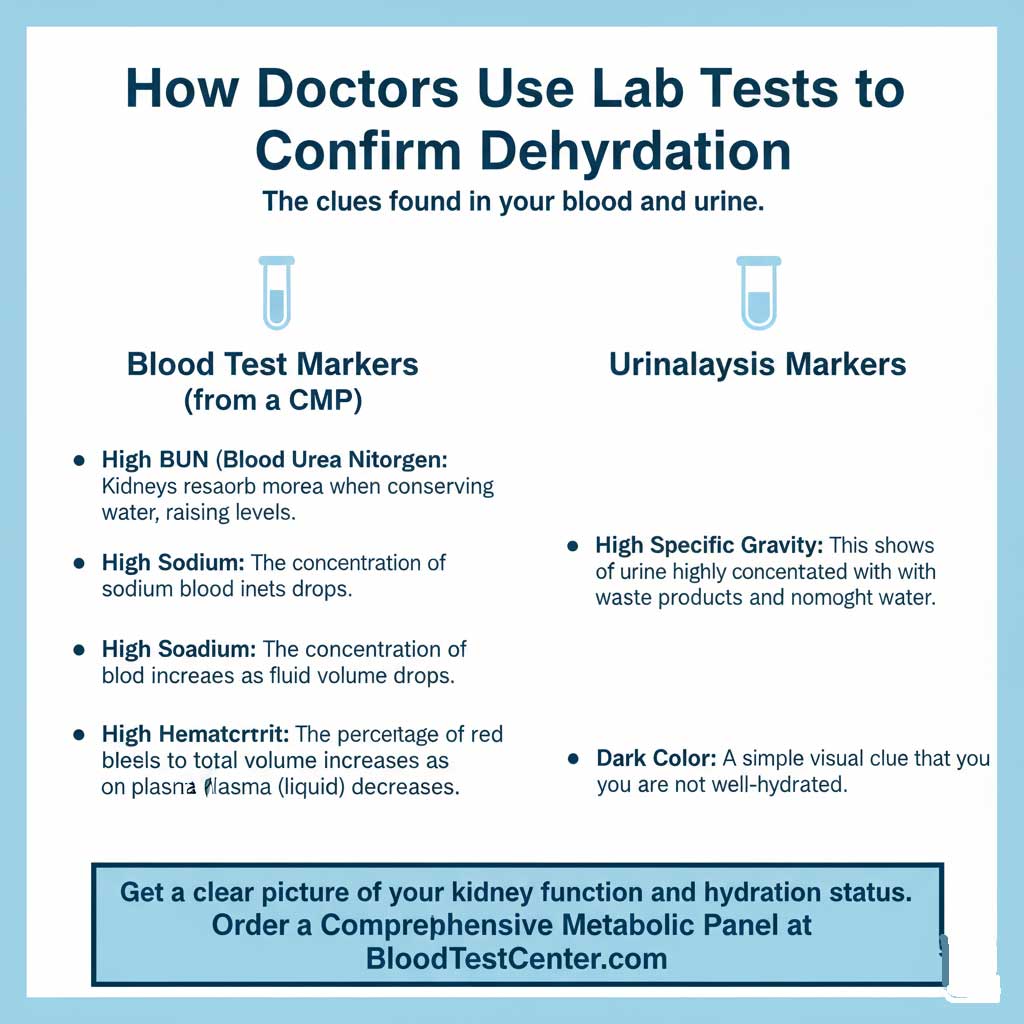
How Doctors Confirm Dehydration is the Cause
Your doctor can use simple and common lab tests to confirm your hydration status, which helps connect the dots between the reading and its cause.
- Blood Tests: A Comprehensive Metabolic Panel (CMP) can reveal several tell-tale signs of dehydration. This includes high BUN levels dehydration, an elevated hematocrit (the percentage of red blood cells to total blood volume), and a high sodium level. The link between dehydration and sodium high blood pressure is a key diagnostic clue.
- Urinalysis: A simple urine test will show highly concentrated urine, measured as a “high specific gravity.”
If your doctor suspects dehydration is affecting your blood pressure, they may order a Comprehensive Metabolic Panel (CMP). You can order this test directly through BloodTestCenter.com to get a clear picture of your kidney function (BUN, creatinine), electrolyte levels, and hydration status before your next appointment.
Treatment in Acute Cases
In a clinical or hospital setting, the fastest and most effective way to treat significant dehydration is with IV fluids for dehydration. Delivering a saline solution directly into the bloodstream bypasses the digestive system and rapidly restores blood volume, which can quickly stabilize a patient’s blood pressure.
Conclusion: Your First, Simplest Step to Better Blood Pressure
So, does dehydration cause high blood pressure? Unquestionably, yes. It triggers a natural but stressful survival response orchestrated by the hormone vasopressin that is specifically designed to raise your blood pressure. While this is a temporary fix, chronic dehydration and hypertension can be linked, as this process forces your cardiovascular system to work harder day after day.
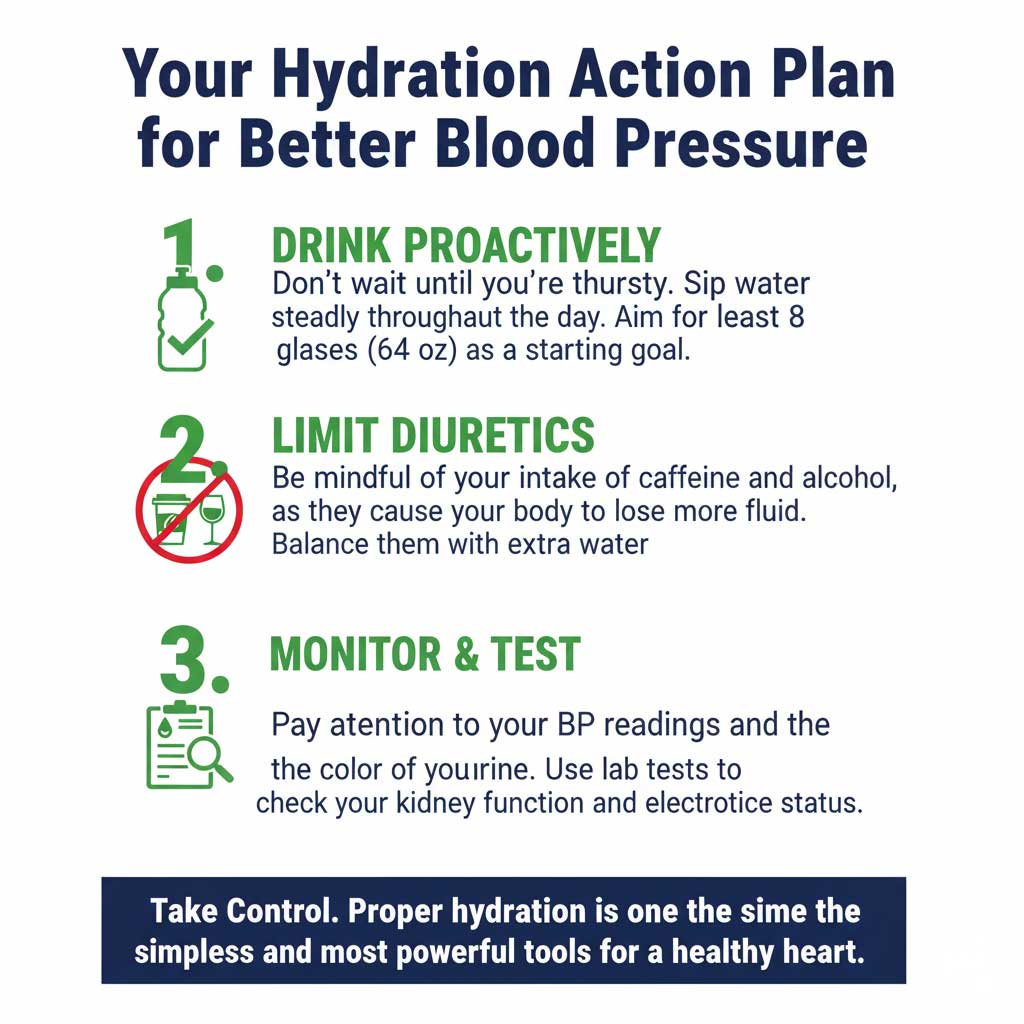
Understanding this connection is empowering. It means that one of the easiest, cheapest, and most accessible lifestyle changes you can make for your heart health is to simply drink enough water. It’s a foundational step that supports everything else you do to maintain a healthy blood pressure.
Start today by tracking your water intake. And if you’re concerned about your blood pressure and want a complete picture of your health—including your hydration status and kidney function—visit BloodTestCenter.com to order your wellness panels. Knowledge is the first step to control.
Frequently Asked Questions (FAQ)
1. Can drinking too much water be dangerous for my blood pressure?
Yes, though it is rare. Drinking an extreme amount of water in a very short time can lead to a condition called hyponatremia (dangerously low sodium levels), which can cause serious health problems. For most people, simply drinking to satisfy thirst and maintain light-colored urine is perfectly safe.
2. If I have high blood pressure, should I drink more water than the recommended amount?
You should aim to consistently meet the recommended daily fluid intake. Drinking more than that is not likely to provide any additional blood pressure-lowering benefit and is generally not necessary unless you are losing extra fluids through sweat.
3. Does the temperature of the water matter for hydration?
No, your body will absorb cold and room temperature water equally well. Some people find it easier to drink more cool water, so choose the temperature that you prefer and that encourages you to drink consistently.
4. Can dehydration cause my blood pressure medication to be less effective?
Dehydration places extra strain on your cardiovascular system, which can make it seem like your medication isn’t working as well. By staying properly hydrated, you are creating an optimal environment for your blood pressure medication to do its job effectively.
5. What are the best foods for staying hydrated?
Many fruits and vegetables have very high water content and can contribute to your daily fluid intake. Excellent choices include watermelon, cucumbers, celery, strawberries, and oranges.
6. How can I tell if a headache is from high blood pressure or just dehydration?
It’s nearly impossible to tell from the headache alone, as they can feel very similar. The best first step is to drink a large glass or two of water. If the headache improves significantly within an hour, it was likely caused by dehydration. If it persists or is severe, it’s important to check your blood pressure and consult a doctor.
7. Can chronic, low-level dehydration lead to permanent hypertension?
Yes, it is considered a significant contributing factor. If your body is constantly in a state of mild dehydration, your cardiovascular system is always working under the strain of the vasopressin response. Over many years, this can contribute to the stiffening of arteries and the development of chronic hypertension.
8. Do I need to drink more water if I’m on a high-protein diet?
Yes. Your kidneys require more water to process the byproducts of protein metabolism, specifically nitrogen. A high-protein diet increases your daily fluid needs to ensure your kidneys can function efficiently without stress.
9. Is thirst a reliable indicator of dehydration?
For many young, healthy adults, it is. However, by the time you feel thirsty, you are already mildly dehydrated. For older adults, the thirst mechanism becomes much less reliable, making it a poor indicator. It’s better to drink proactively throughout the day rather than waiting for thirst to strike.
10. What’s the best way to rehydrate safely if I already have high blood pressure?
The best way is to drink plain water steadily throughout the day rather than chugging a large amount at once. Avoid sugary drinks and be mindful of the sodium content in sports drinks. If your doctor has you on a fluid-restricted diet for a condition like heart failure, it is essential to follow their specific instructions.