You stand up too quickly on a hot day and the room suddenly spins. You experience a wave of fatigue and nausea in the middle of a workout that you can’t seem to shake. These unsettling moments of dizziness and lightheadedness are incredibly common, and while we might blame them on stress or lack of sleep, one of the most direct causes is often overlooked: dehydration.
Table of Contents
The question is a critical one for your health and safety: Does dehydration cause low blood pressure? The answer is a definitive yes. In fact, significant dehydration is one of the most common and direct causes of a sudden, symptomatic drop in blood pressure, a condition known medically as hypotension.
This comprehensive guide from BloodTestCenter.com will explore the critical link between your fluid intake and your blood pressure. Understanding how a lack of water can lead to a drop in dehydration and blood volume, overwhelm your body’s coping mechanisms, and cause dangerous hypotension is the first step toward preventing it.
The Fundamental Connection: How Dehydration Reduces Blood Volume
To understand how dehydration and low blood pressure are linked, it’s essential to first understand the composition of your blood. The science is simple but profound.
Your Blood is Mostly Water
Your blood is not just a collection of cells; it is a fluid suspension. The liquid component, called plasma, makes up more than half of your blood’s total volume, and that plasma is about 92% water. This means your total dehydration and blood volume is directly and immediately dependent on your hydration status.
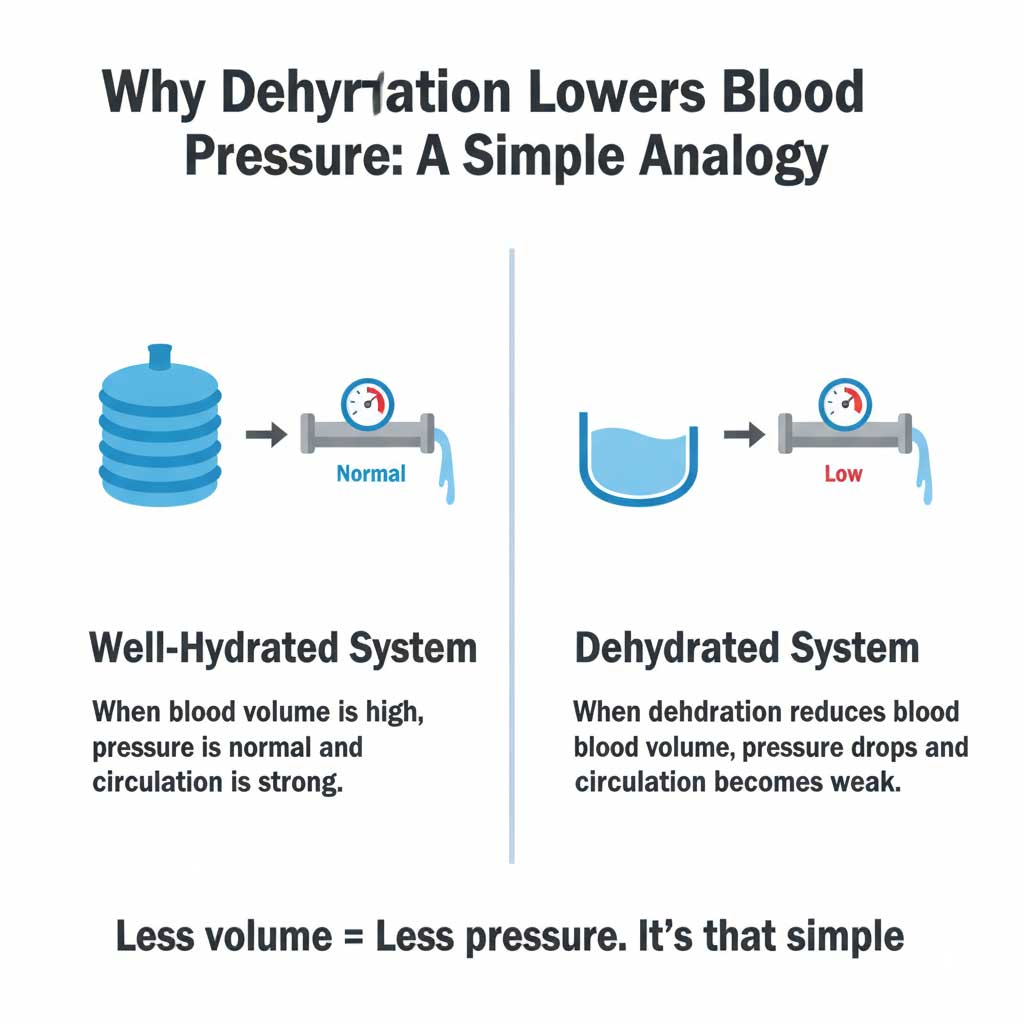
The Plumbing Analogy
Think of your circulatory system like the plumbing in a house. If you were to drain half the water out of the central tank, the water pressure coming out of every faucet would drop significantly. Your cardiovascular system works on the exact same principle. When you lose more fluid than you take in—through sweat, urine, breathing, vomiting, or diarrhea—your body scrambles to maintain its essential functions. It begins to pull water from various tissues, including from your bloodstream, to support your organs. This directly reduces the total volume of blood in your arteries and veins. With less fluid pushing against the arterial walls, the pressure inside them inevitably falls.
The Blood Pressure Paradox: Why Dehydration Can Cause BOTH High and Low Readings
One of the most confusing aspects of this topic is the question of high vs low blood pressure dehydration. You may have read that dehydration can raise blood pressure, so how can it also cause it to drop? The answer lies in understanding that your body’s response to dehydration happens in distinct stages.
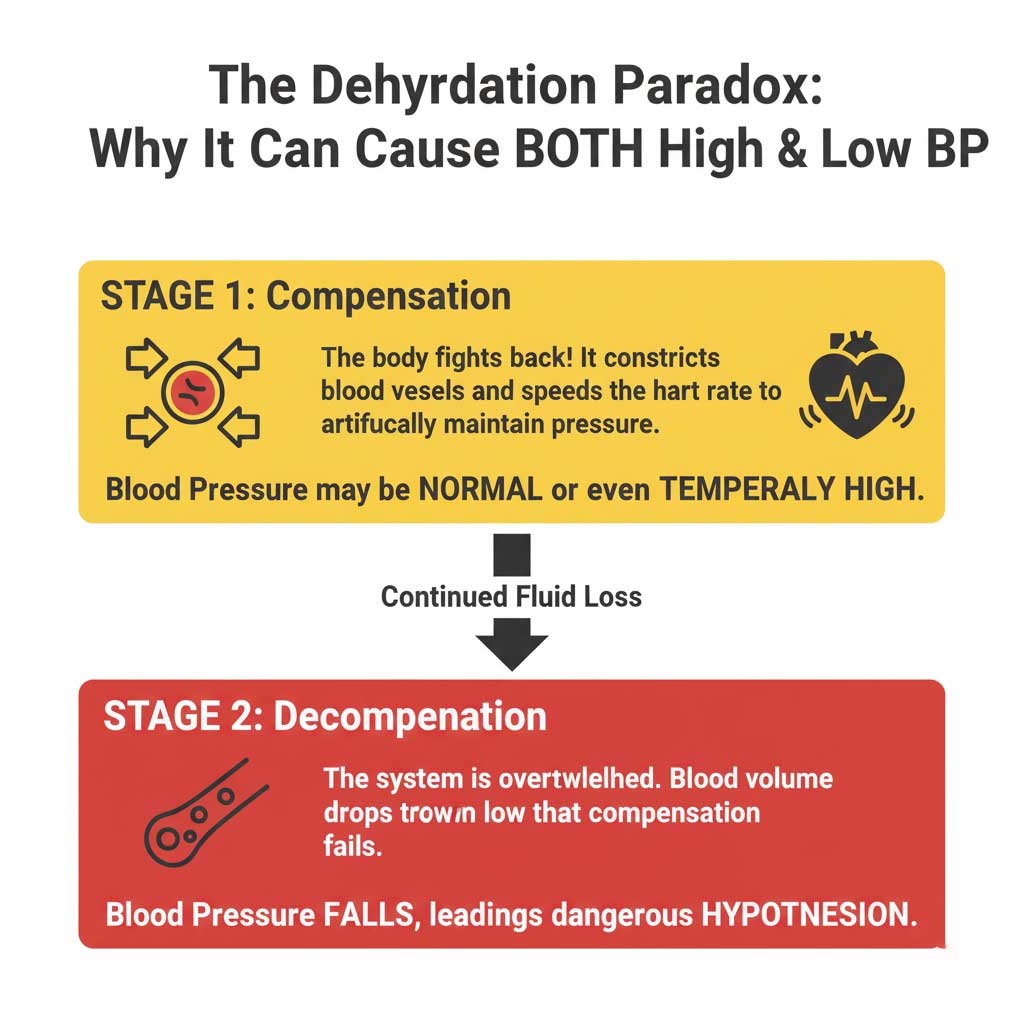
Stage 1: The Compensation Phase (Normal or HIGH BP)
In the initial stages of mild to moderate dehydration, your body activates a brilliant and powerful defense mechanism to prevent a dangerous drop in blood pressure.
- Your brain detects the low fluid volume and releases hormones, most notably vasopressin and angiotensin.
- These hormones cause your smaller blood vessels to constrict (a process called vasoconstriction). This narrowing of the “pipes” artificially increases the pressure inside them.
- At the same time, your heart begins to beat faster (tachycardia) to circulate the limited blood more rapidly.
During this compensation phase, your body is fighting hard to keep blood flowing to your brain and heart. As a result, your blood pressure reading might be perfectly normal or even temporarily high. This is the body’s way of sounding the alarm that it needs fluid.
Stage 2: The Decompensation Phase (LOW BP – Hypotension)
If the fluid loss continues and you don’t rehydrate, the body’s compensation system eventually gets overwhelmed and fails. The dehydration and blood volume drops so severely that there simply isn’t enough fluid left in the system to maintain pressure, no matter how hard the heart pumps or how constricted the blood vessels become.
At this point, you enter the decompensation phase, and your blood pressure begins to fall. This is when clinical hypotension sets in, and the dangerous and noticeable symptoms begin to appear.
Recognizing the Red Flags: Symptoms and Key Signs
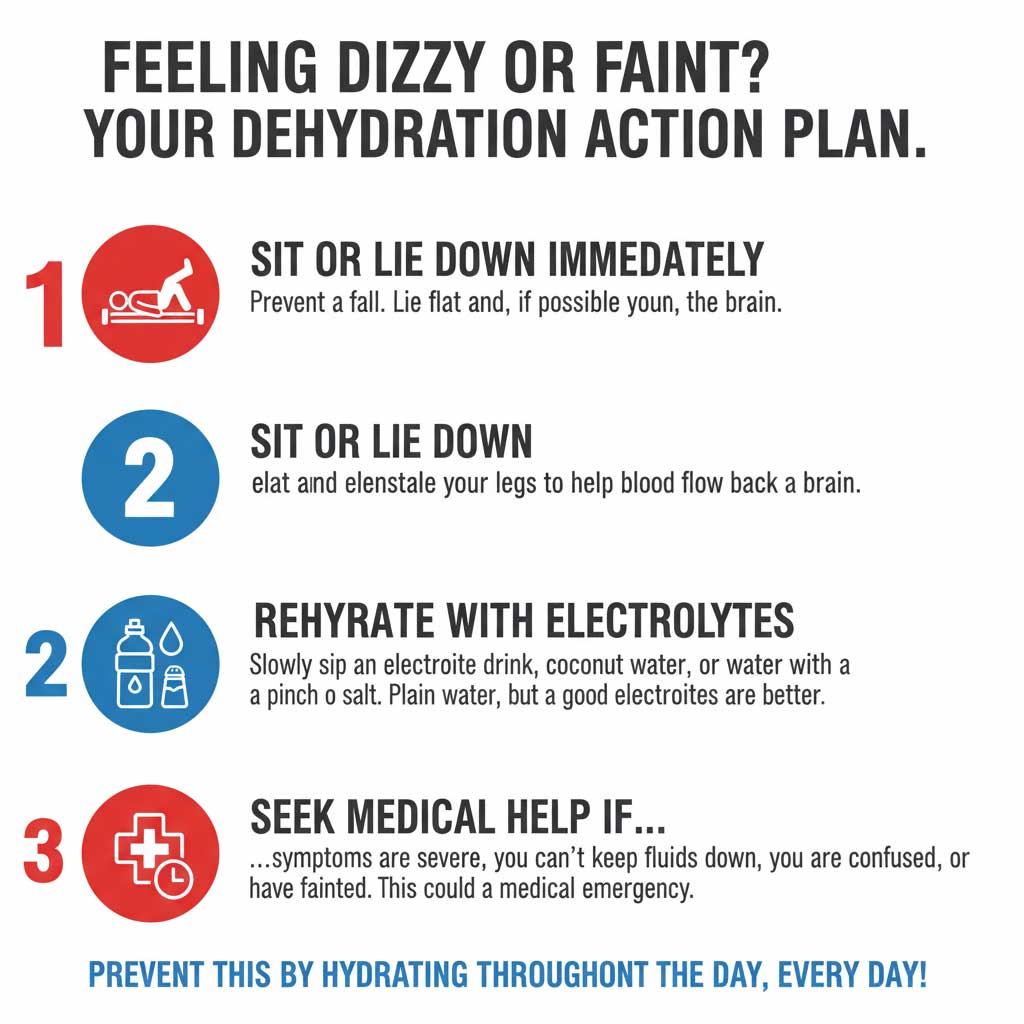
The symptoms of low blood pressure from dehydration are a direct result of your brain and other vital organs not receiving enough oxygen-rich blood. It’s crucial to recognize these signs early.
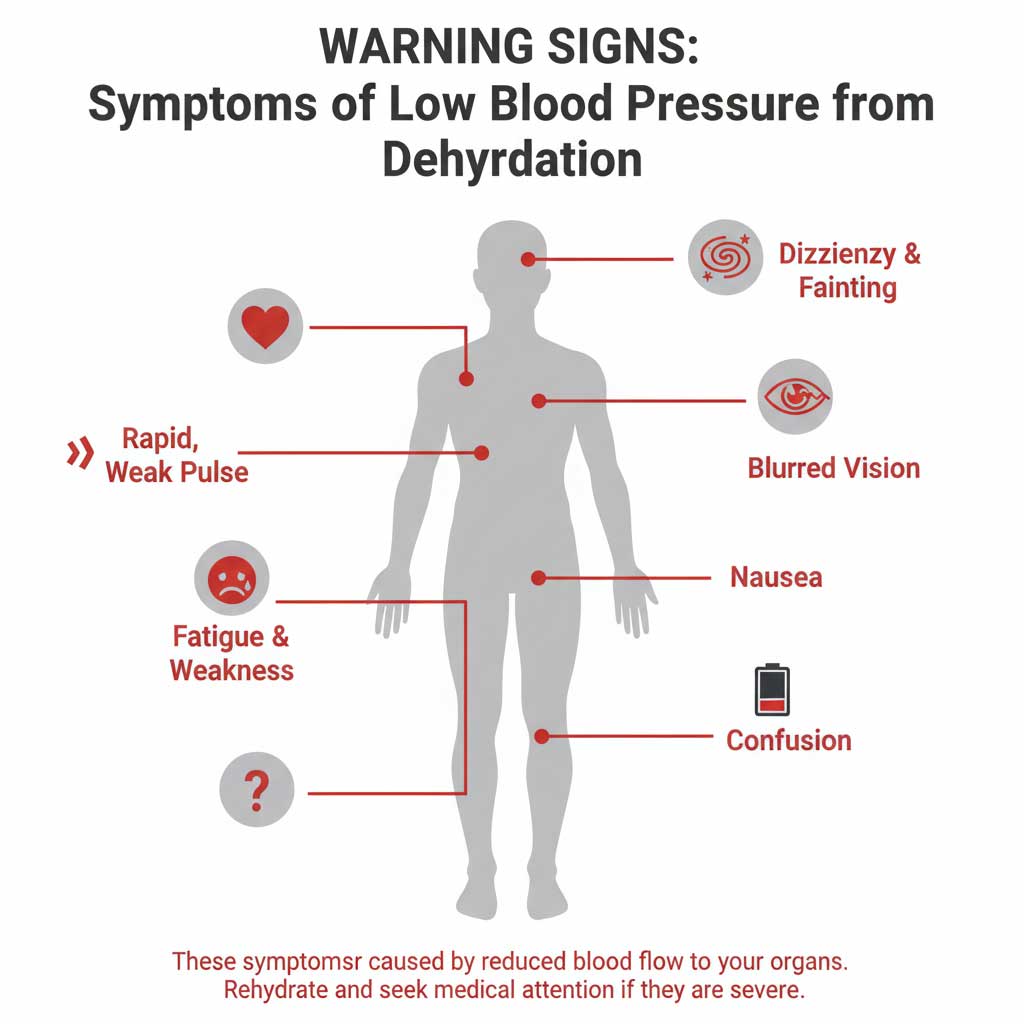
The Classic Symptoms of Low Blood Pressure from Dehydration
- Dizziness and lightheadedness, which are often the first signs.
- Fainting (the medical term is syncope).
- Profound fatigue and a feeling of heavy weakness.
- Nausea.
- Blurred vision.
- Confusion or difficulty concentrating.
Orthostatic Hypotension: The “Head Rush” Explained
One of the hallmark symptoms is orthostatic hypotension dehydration. This is the medical term for the sharp feeling of dizziness or faintness that occurs when you change positions, especially from lying down or sitting to standing up.
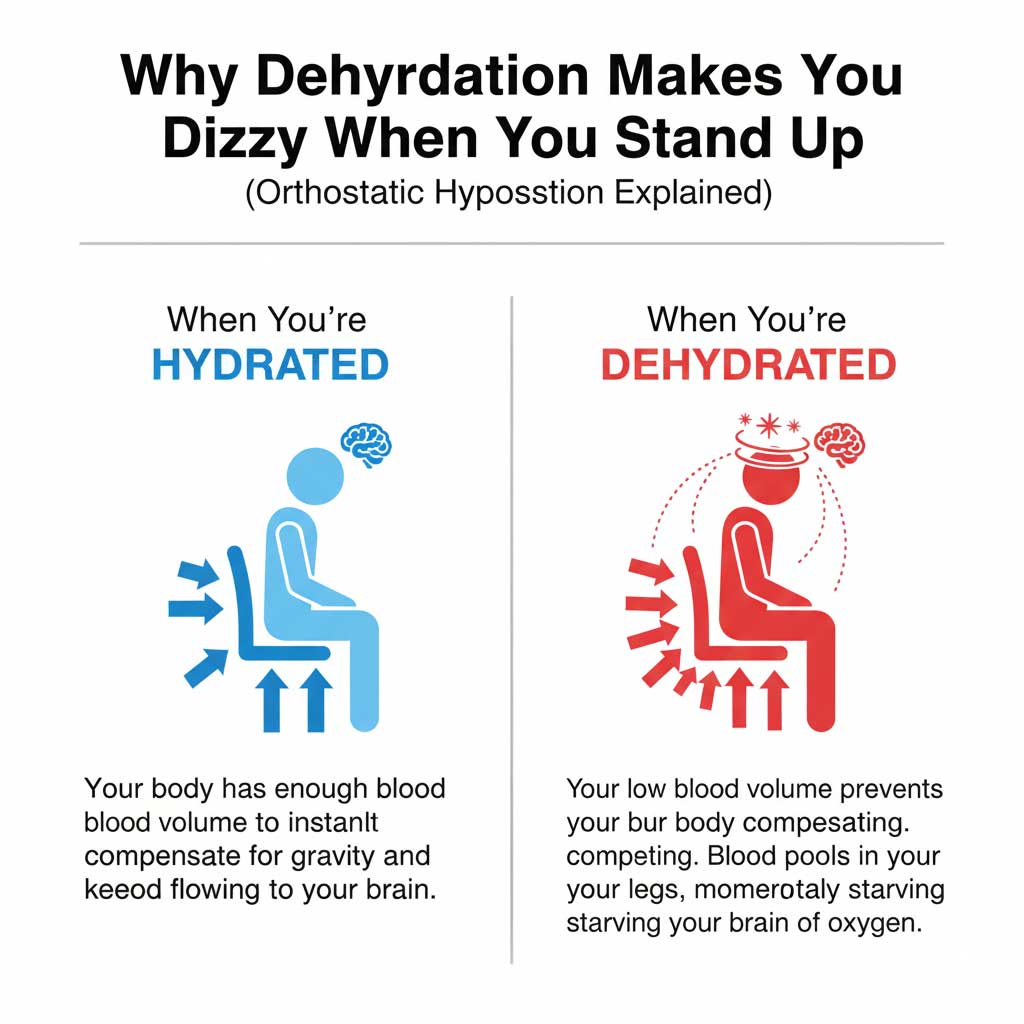
When you stand, gravity naturally pulls blood down into your legs and abdomen. A healthy, well-hydrated body instantly counteracts this by constricting blood vessels and increasing the heart rate to push blood back up to the brain. When you’re dehydrated, this response is sluggish and ineffective. Blood pools in your lower body, and your brain is momentarily starved of blood flow, causing that intense “head rush” or feeling that you might pass out.
Low Blood Pressure and a Rapid Heart Rate: The Telltale Combo
A key diagnostic clue for medical professionals is the combination of dehydration low blood pressure rapid heart rate. As your blood pressure falls, your heart speeds up in a desperate attempt to compensate by pumping the small amount of remaining blood faster. If you feel dizzy and your pulse is fast and weak, it’s a strong indicator of significant dehydration.
Hypovolemic Shock: The Ultimate Danger
If dehydration becomes severe and is not treated, it can progress to hypovolemic shock. This is a life-threatening medical emergency where the loss of blood volume is so extreme that the heart can no longer pump enough blood to sustain organ function. The symptoms include all of those listed for hypotension, but they become more severe and are often accompanied by rapid, shallow breathing, pale, cold, and clammy skin, and eventual loss of consciousness. Hypovolemic shock requires immediate 911 intervention.
Who is Most at Risk? Identifying Vulnerable Populations
While anyone can experience dehydration and low blood pressure, certain groups are far more susceptible.
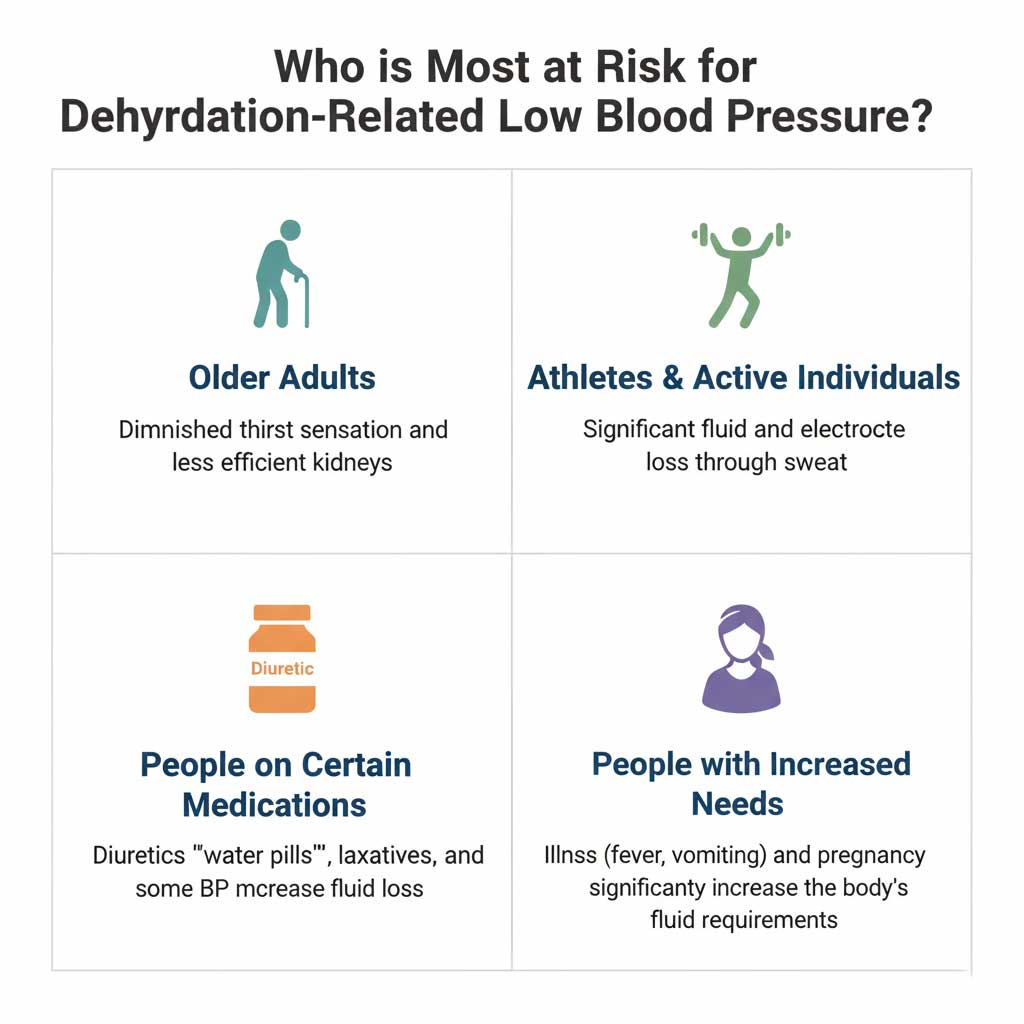
- Older Adults: The elderly are a major high-risk group. Their natural thirst mechanism often becomes less sensitive with age, and their kidneys may be less efficient at conserving water.
- Athletes and Outdoor Workers: Anyone who sweats profusely is at risk. It’s common to experience low blood pressure after exercise if fluid and electrolyte losses are not adequately replaced.
- People on Certain Medications: Diuretics and dehydration are a common combination. Diuretics, or “water pills,” are often prescribed for high blood pressure and work by forcing the body to excrete sodium and water. This makes users highly vulnerable to dehydration and subsequent hypotension.
- Pregnant Women and Children: Pregnant women have increased fluid needs, and children have a higher body surface area to volume ratio, making them lose fluid more quickly, especially when ill.
Diagnosis and Treatment: Restoring Volume and Pressure
If you present to a doctor with symptoms of hypotension, they will work quickly to determine if dehydration is the cause.
How Doctors Confirm the Diagnosis
The diagnostic process is typically straightforward and involves:
- Physical Exam: The doctor will check your blood pressure and heart rate while you are lying down and then again after you stand up to test for orthostatic hypotension dehydration.
- Lab Tests: Blood and urine tests are essential for confirming the diagnosis.
- BloodTestCenter.com Integration: To confirm dehydration, a doctor will often order a Basic or Comprehensive Metabolic Panel (BMP or CMP). You can order these tests directly through BloodTestCenter.com to get a clear picture of your hydration status. The results will often show key signs like a high BUN (Blood Urea Nitrogen) to creatinine ratio, abnormal electrolyte levels (sodium and potassium), and a high hematocrit, all of which point to a low fluid volume and the cause of your hypotension.
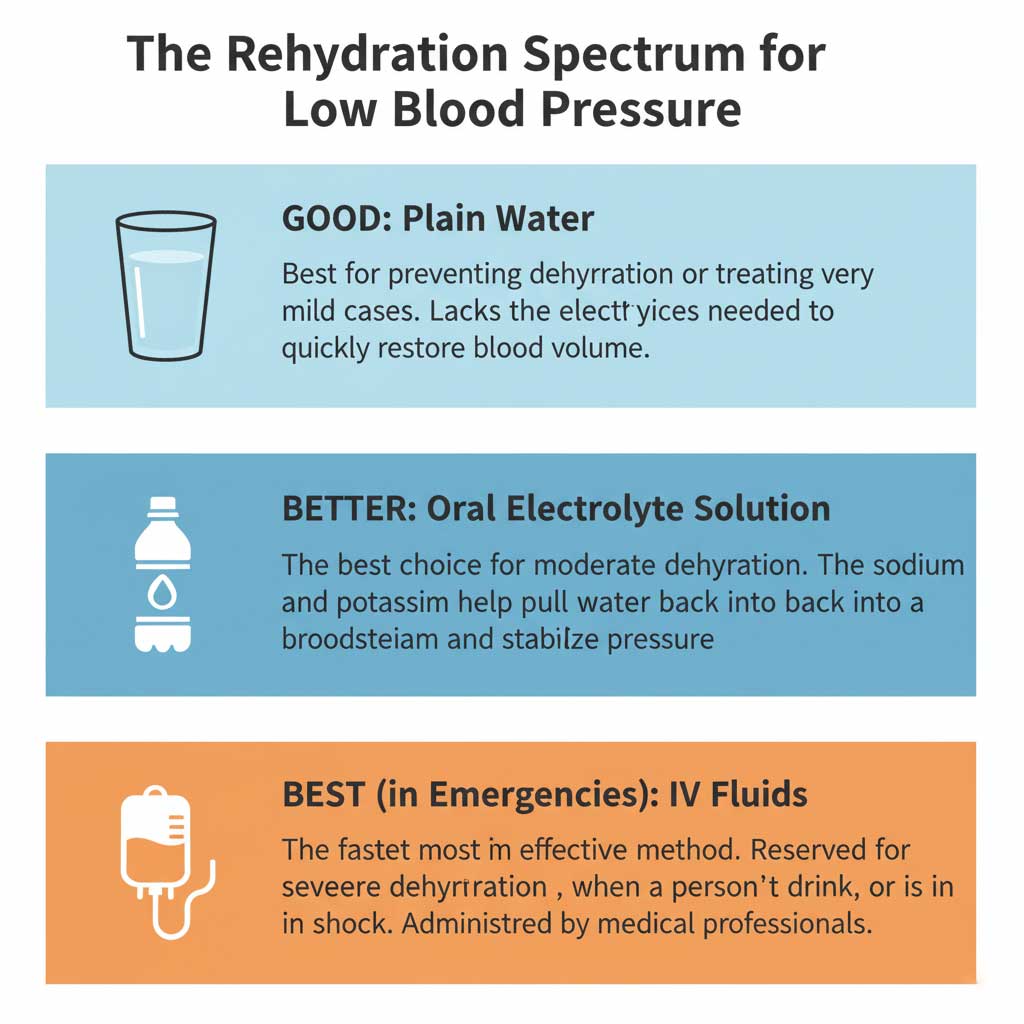
The Rehydration Strategy
The treatment for dehydration and low blood pressure is, simply, rehydration. However, the method matters. In cases of significant fluid loss, plain water may not be enough. Electrolyte drinks for low blood pressure are often a better choice because they contain sodium, which is the key electrolyte that helps your body pull water back into the bloodstream and, more importantly, keep it there.
| Rehydration Method | Description | Best For… | Speed of BP Normalization |
| Plain Water | Simple fluid replacement. Does not contain electrolytes. | Mild Dehydration or for prevention. It can quench thirst but may not be enough to quickly restore blood volume if electrolytes are low. | Slow to Moderate. Can take several hours as the body needs electrolytes to retain the water effectively in the bloodstream. |
| Oral Electrolyte Solution (e.g., Pedialyte, sports drinks) | Contains a balanced mix of water, sodium, potassium, and glucose designed for rapid absorption and fluid retention. | Moderate Dehydration. Ideal for situations involving significant sweat, vomiting, or diarrhea. The gold standard for oral rehydration. | Moderate to Fast. Can begin to stabilize blood pressure within an hour or two as electrolytes help restore intravascular volume. |
| Intravenous (IV) Fluids | A sterile saline and electrolyte solution administered directly into a vein by a medical professional. | Severe Dehydration. Used when a person cannot keep fluids down, is confused, or is in or near hypovolemic shock. | Immediate and Rapid. The fastest way to raise blood pressure from dehydration, with effects seen within minutes. This is the standard in emergency medicine. |
With oral rehydration, symptoms can begin to improve within an hour, but it can take several hours for blood pressure to fully stabilize. With IV fluids for dehydration, the improvement is much more rapid.
Conclusion: Hydration is a Pillar of Blood Pressure Stability
So, does dehydration cause low blood pressure? Unquestionably, yes. It is a direct and common cause of hypotension. By reducing your blood volume to a point where your body’s clever coping mechanisms fail, it creates a dangerous situation that can lead to dizziness, fainting, and in severe cases, life-threatening hypovolemic shock.
Understanding this connection is empowering. It means that paying close attention to your hydration status is a fundamental and non-negotiable part of managing your cardiovascular health. Proper hydration is a pillar of blood pressure stability.
Pay attention to the early signs of dehydration and take action by rehydrating, preferably with electrolyte-rich fluids. If you experience persistent or severe symptoms of low blood pressure from dehydration, it’s crucial to seek medical attention. Don’t guess about the cause. Visit BloodTestCenter.com to order the tests that can give you and your doctor the data needed for a clear diagnosis and a plan to get you back on your feet.
Frequently Asked Questions (FAQ)
1. Is it dangerous if I faint from dehydration?
Yes, can dehydration cause fainting is a serious sign. While a single fainting spell may not cause lasting harm, it indicates significant dehydration. Furthermore, the act of fainting can lead to injuries from falls, such as head trauma. It should always be taken seriously.
2. What’s the best thing to drink immediately if I feel dizzy from dehydration?
An oral rehydration solution that contains both electrolytes and a small amount of sugar is ideal. If that’s not available, a sports drink or even a glass of water with a pinch of salt and sugar can be more effective than plain water alone.
3. How can I tell if my heart is racing because of anxiety or dehydration?
It can be difficult to tell from the sensation alone, as they can feel similar. However, a rapid heart rate from dehydration is often accompanied by other physical symptoms like dizziness upon standing, dry mouth, and dark urine. Anxiety may be accompanied by feelings of worry or panic.
4. Can chronic dehydration cause me to have low blood pressure all the time?
It’s less common for chronic dehydration to cause persistent low blood pressure. More often, chronic low-level dehydration keeps the body in the “compensation phase,” which can contribute to long-term high blood pressure. Episodes of low blood pressure are more typical of acute, significant dehydration.
5. Why do I feel better after eating something salty when I’m dehydrated?
When you are dehydrated from sweating, you lose both water and salt (sodium). Eating something salty helps replenish the lost sodium. Sodium is crucial for holding water in your bloodstream, which helps to restore blood volume and, consequently, your blood pressure.
6. Can you have symptoms of dehydration even if you don’t feel thirsty?
Absolutely. This is especially true for older adults, whose thirst mechanism becomes less reliable. By the time you feel thirsty, you are already dehydrated. It’s better to drink proactively throughout the day.
7. Does coconut water work as an electrolyte drink for low blood pressure?
Coconut water is a good source of potassium but is relatively low in sodium compared to commercial oral rehydration solutions. It can be helpful for mild dehydration but may not be sufficient for replacing the sodium lost during intense sweating or illness.
8. Can my blood pressure fluctuate a lot during the day if I’m dehydrated?
Yes. Dehydration and low blood pressure can cause significant fluctuations, especially when you change positions. Your blood pressure might be near-normal when you are lying down but drop sharply when you stand up, leading to a feeling of instability.
9. What does the Mayo Clinic or American Heart Association say about this?
Both the Mayo Clinic dehydration hypotension link and the American Heart Association recognize dehydration as a clear cause of low blood pressure. They emphasize that in severe cases, it can lead to hypovolemic shock, a medical emergency.
10. If I have low blood pressure, should I drink more fluids than someone with high blood pressure?
Not necessarily. Everyone should aim for adequate daily hydration. If you have a chronic tendency toward low blood pressure, ensuring you are consistently well-hydrated is a critical part of your management plan to prevent symptomatic drops in pressure.

