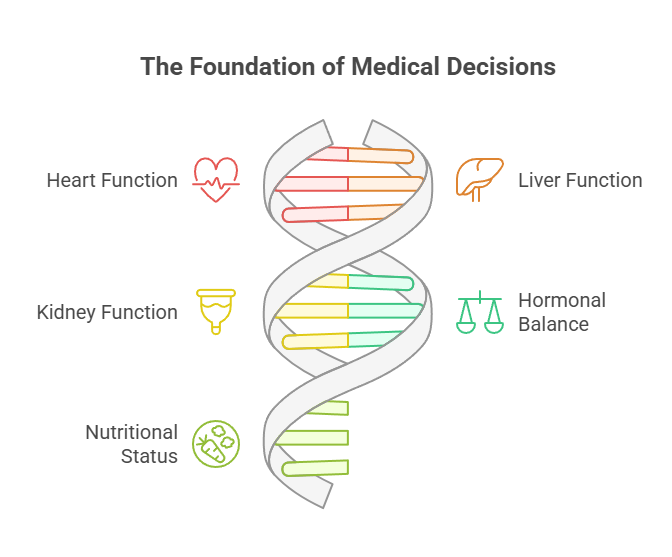
In the landscape of modern medicine, the humble blood test stands as a titan of diagnostics. It is your personal biochemical snapshot, a window into the intricate workings of your body that provides your doctor with invaluable information. From the function of your heart, liver, and kidneys to your hormonal balance and nutritional status, these tests form the bedrock of countless medical decisions. They are the silent arbiters that guide diagnoses, monitor the effectiveness of treatments, screen for disease long before symptoms appear, and ultimately, safeguard your health.
But what if this critical snapshot was distorted? What if the very substances you take to manage your health—your daily prescriptions, your over-the-counter pain relievers, even your “all-natural” vitamins—were silently sabotaging the accuracy of your results?
This is not a fringe possibility; it is a daily reality in clinical practice, and its consequences can be severe. An inaccurate lab result can trigger a domino effect of negative outcomes: a life-threatening condition like heart disease or a thyroid disorder being missed entirely; a false diagnosis leading to unnecessary prescriptions with their own side effects and costs; or the profound anxiety and stress that comes from trying to make sense of confusing and contradictory medical data.
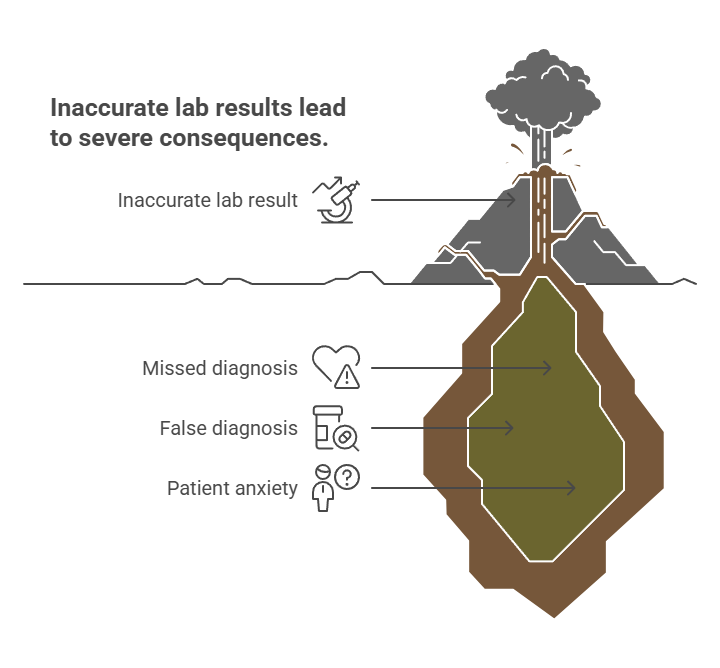
The power to prevent this chaos rests in knowledge. To transform yourself from a passive subject of a blood draw into a proactive, empowered guardian of your own health data, you must understand the hidden world of drug-laboratory test interactions. This definitive guide is designed to give you that power. We will delve deeper than ever before into how and why these interferences happen, exposing the culprits in every corner of your medicine cabinet and giving you the actionable tools you need to ensure your next blood test is as accurate as humanly possible.
Understanding the Two Faces of Interference
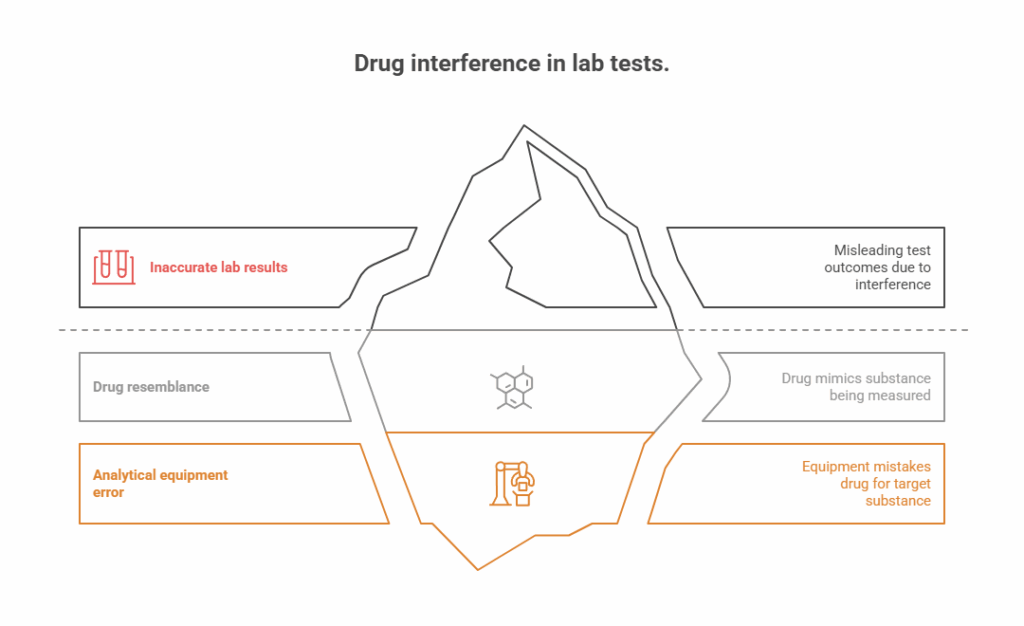
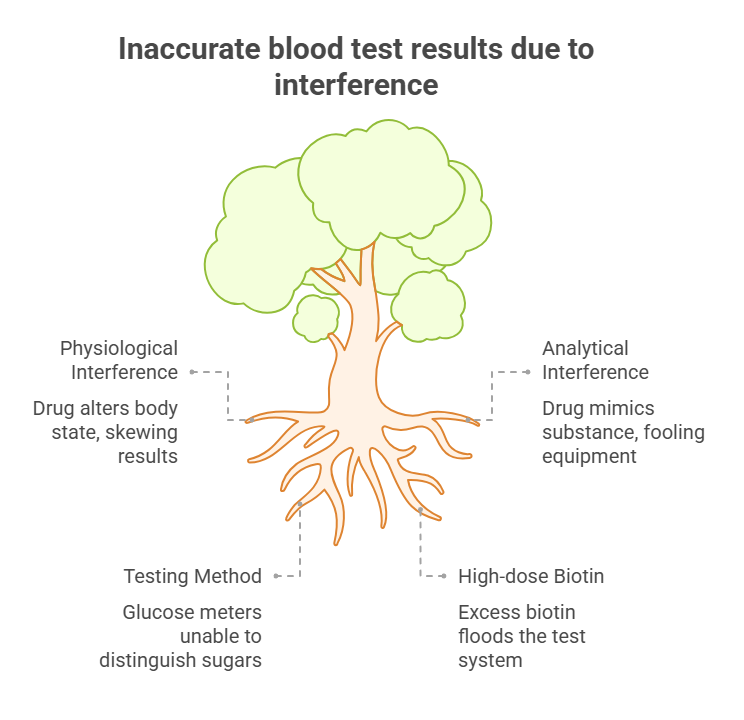
When a medication or supplement alters a lab test, it’s not a single, simple event. The interference happens in one of two fundamentally different ways: by changing your body’s physiology or by fooling the lab’s machinery. Understanding the distinction is key to grasping the whole picture.
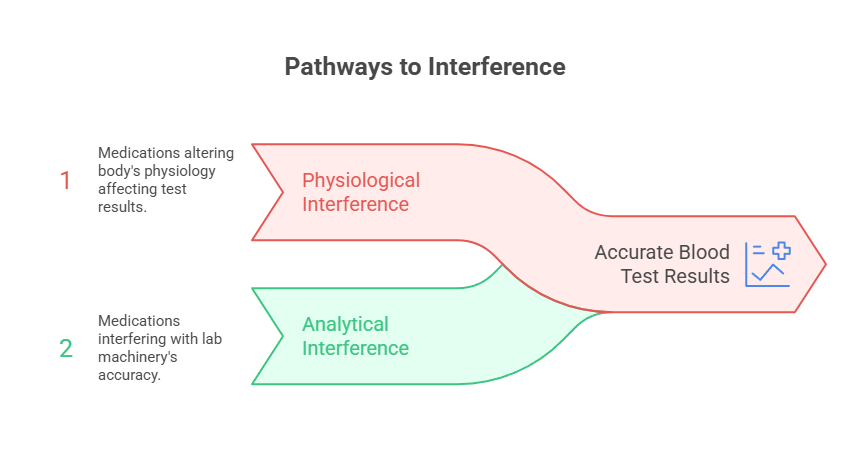
Physiological Interference (The In Vivo Effect)
This is the most common form of interaction. It occurs when a substance causes a real, biological change in your body, altering the level of the substance being measured. The laboratory test is performing its job perfectly—it is accurately measuring the concentration of the marker in your blood. However, that concentration has been artificially pushed up or down by the medication you’re taking.
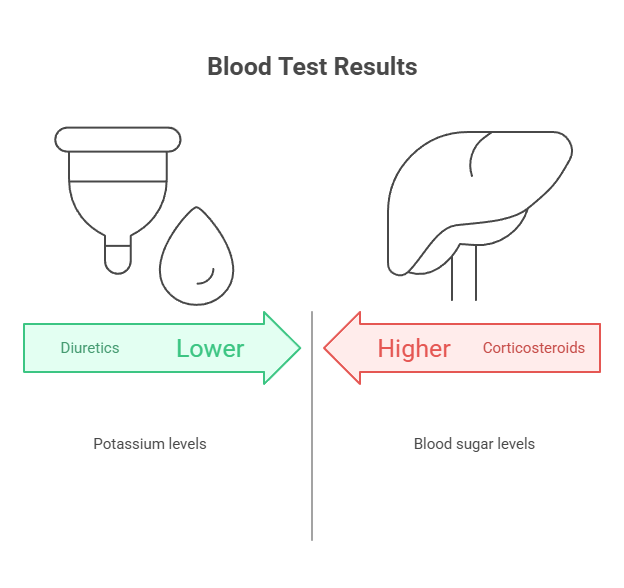
- Classic Example: Corticosteroids and Blood Sugar. When you take a steroid like prednisone, it can stimulate your liver to produce more glucose and can make your body’s cells more resistant to insulin. A blood test will, therefore, show genuinely higher blood sugar levels. The test is accurate, but the result is a direct, physiological consequence of the drug, which could be mistaken for pre-diabetes or poor diabetic control if the context is ignored.
- Classic Example: Diuretics and Potassium. A diuretic (or “water pill”) like furosemide works by making your kidneys excrete more sodium, and water follows. In this process, your kidneys also excrete more potassium. A blood test will correctly show lower potassium levels. Again, the test is not wrong; it’s measuring a real, drug-induced change in your body’s chemistry.
Analytical Interference (The In Vitro Effect)
This mechanism is more insidious. It happens inside the test tube, when the drug itself—or a metabolite your body creates from it—chemically or structurally resembles the substance the lab is trying to measure. It essentially wears a disguise, tricking the highly sensitive analytical equipment into a case of mistaken identity. In this scenario, the lab result does not reflect your body’s true state at all.
- Classic Example: Antibiotics and Glucose Meters. Some older generations of hospital glucose meters used a testing method (GDH-PQQ) that couldn’t distinguish between glucose and certain other sugars, like maltose. Some intravenous antibiotics contain maltose. This led to tragic cases where patients on these antibiotics were given dangerously high doses of insulin based on falsely astronomical glucose readings.
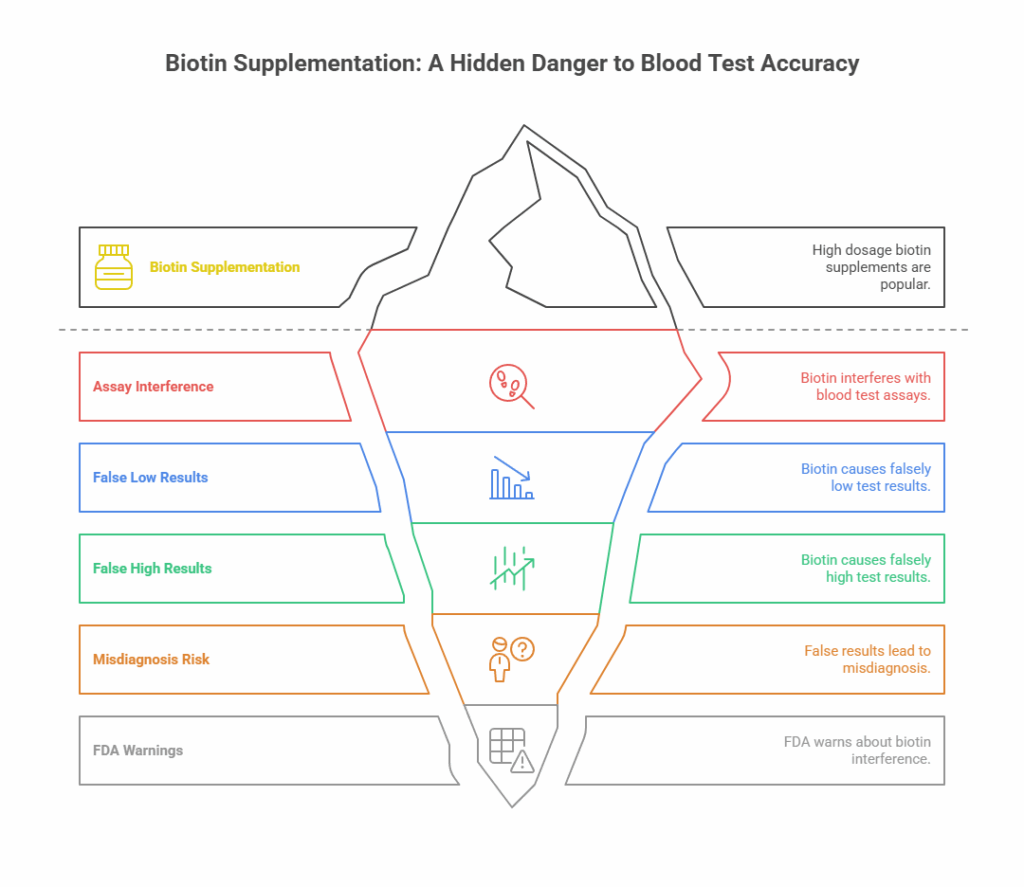
- The Modern Poster Child: Biotin. As we will explore in-depth, many of the most advanced and common lab tests today rely on a “biotin-streptavidin” binding system. When a patient takes high-dose biotin supplements, the excess biotin floods the test system, directly interfering with the analytical machinery and producing wildly inaccurate results for dozens of critical tests.
Prescription Medications – A Deep Dive into Common Culprits
It is imperative to begin this section with a critical warning: Under no circumstances should you ever stop taking a prescribed medication without the explicit guidance of the healthcare provider who prescribed it. These drugs are often life-sustaining. The goal is not to stop them, but to understand their known effects so your results can be interpreted correctly.
The Cardiovascular Drug Cabinet
Medications for heart health and blood pressure are among the most prescribed in the world, and their effects on blood chemistry are well-documented.
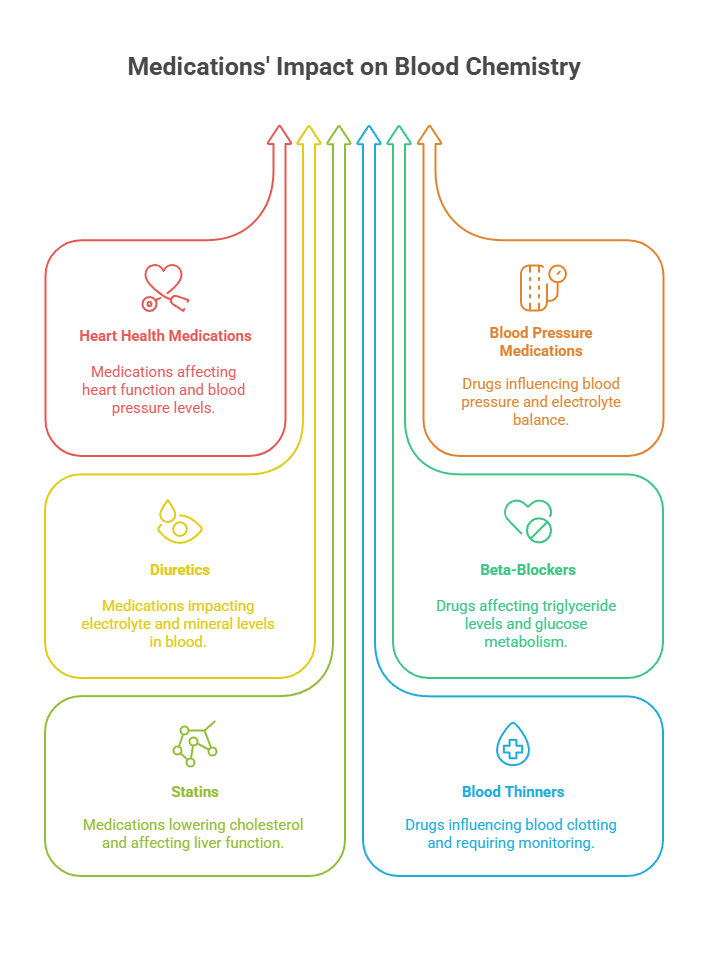
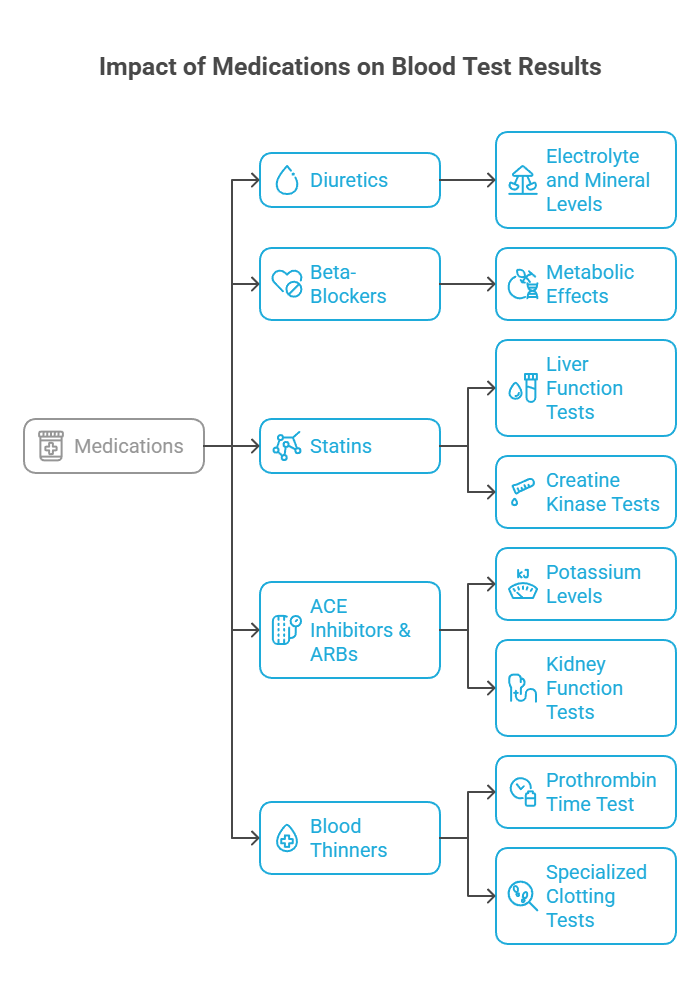
- Diuretics (Hydrochlorothiazide, Furosemide, Spironolactone): As mentioned, these directly impact electrolyte and mineral levels. They are known to decrease potassium, sodium, and magnesium, while potentially increasing calcium and uric acid (which can trigger gout). Doctors order these tests to monitor these expected effects.
- Beta-Blockers (Metoprolol, Atenolol, Carvedilol): These can have metabolic effects. They are known to potentially raise triglyceride levels and lower levels of HDL (“good”) cholesterol. They can also affect glucose metabolism and mask some of the warning signs of low blood sugar in diabetics.
- Statins (Atorvastatin, Rosuvastatin, Simvastatin): The primary purpose of these drugs is to lower LDL (“bad”) cholesterol, so a lipid panel will reflect this. However, doctors also test for two key side effects:
- Liver Function (ALT/AST): To ensure the statin isn’t causing liver inflammation.
- Creatine Kinase (CK): To check for muscle inflammation or breakdown (rhabdomyolysis), a rare but serious side effect.
- ACE Inhibitors & ARBs (Lisinopril, Losartan, Valsartan): These blood pressure medications can cause the body to retain potassium. Therefore, a doctor will monitor potassium levels to prevent hyperkalemia (dangerously high potassium), especially when first starting the drug or in patients with kidney disease. They also monitor kidney function (BUN, creatinine).
- Blood Thinners (Warfarin, Eliquis, Xarelto): For warfarin, the Prothrombin Time (PT/INR) test is not interfered with by the drug; the test exists solely to measure the drug’s effect and guide dosing. For newer direct oral anticoagulants (DOACs), routine monitoring isn’t always required, but they will affect specialized clotting tests.
Hormonal, Endocrine, and Metabolic Medications
This class of drugs is designed to directly manipulate the body’s chemistry.
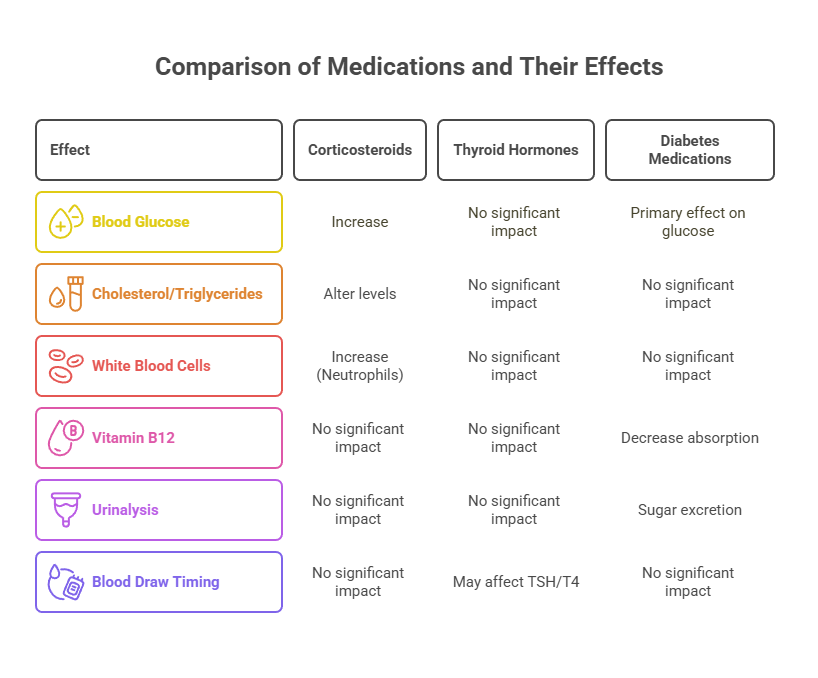
- Corticosteroids (Prednisone, Dexamethasone, Hydrocortisone): These powerful anti-inflammatory drugs have widespread effects. They reliably raise blood glucose, can alter cholesterol and triglyceride levels, and can cause an increase in the number of white blood cells (neutrophils), which can be mistaken for an infection.
- Thyroid Hormones (Levothyroxine, Liothyronine): These are hormone replacements. The TSH and Free T4 tests are done specifically to see if the dose is correct. Taking levothyroxine right before a blood draw can sometimes lead to a temporarily lower TSH and higher T4, so many endocrinologists advise patients to wait until after the test to take their daily pill for the most stable reading.
- Diabetes Medications (Metformin, GLP-1 Agonists, SGLT2 Inhibitors): While their primary effect on glucose is the goal, they have other effects. Metformin is famously associated with decreased Vitamin B12 absorption over the long term, so a B12 level should be checked periodically. SGLT2 inhibitors (like Jardiance) work by making you excrete sugar in your urine, so a urinalysis will reflect this.
Central Nervous System (CNS) Medications
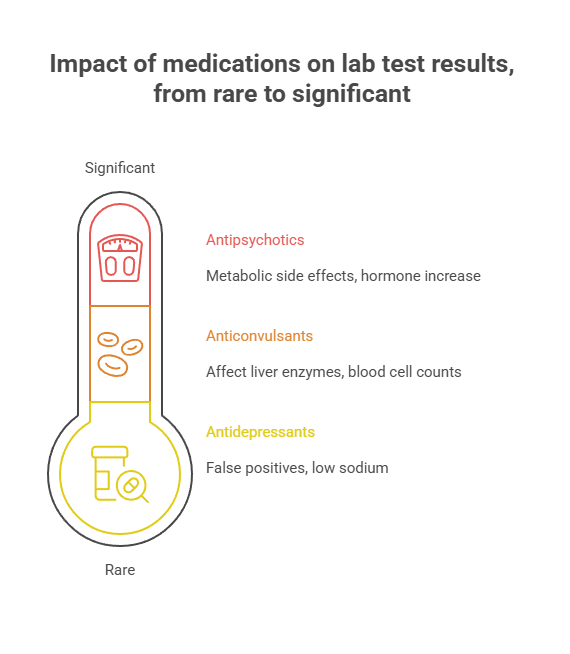
Drugs for mental health and neurological conditions can also impact lab work.
- Antidepressants: Selective Serotonin Reuptake Inhibitors (SSRIs) and others can, in rare cases, lead to a condition called SIADH that causes dangerously low sodium levels. Tricyclic antidepressants (like amitriptyline) have a chemical structure that can sometimes cause a false positive on urine drug screens for phencyclidine (PCP).
- Antipsychotics (Olanzapine, Risperidone): Many drugs in this class are known to have significant metabolic side effects, including weight gain, increased blood glucose, and elevated cholesterol/triglyceride levels. They can also increase levels of the hormone prolactin.
- Anticonvulsants (Carbamazepine, Phenytoin, Valproic Acid): Many older seizure medications can affect liver enzymes and require monitoring of blood cell counts.
The “Natural” Deception – How Vitamins & Herbs Wreak Havoc
One of the most dangerous misconceptions in health is that “natural” equals “safe” or “inert.” Nothing could be further from the truth when it comes to lab testing. Your body metabolizes herbal supplements just like pharmaceuticals, and they can have profound physiological and analytical effects.
The Ultimate Case Study: Biotin (Vitamin B7) – Public Enemy #1 in the Lab
If a single supplement could be crowned king of lab interference, it would be biotin. Its story is a perfect storm of clever marketing, consumer demand, and unintended analytical consequences.
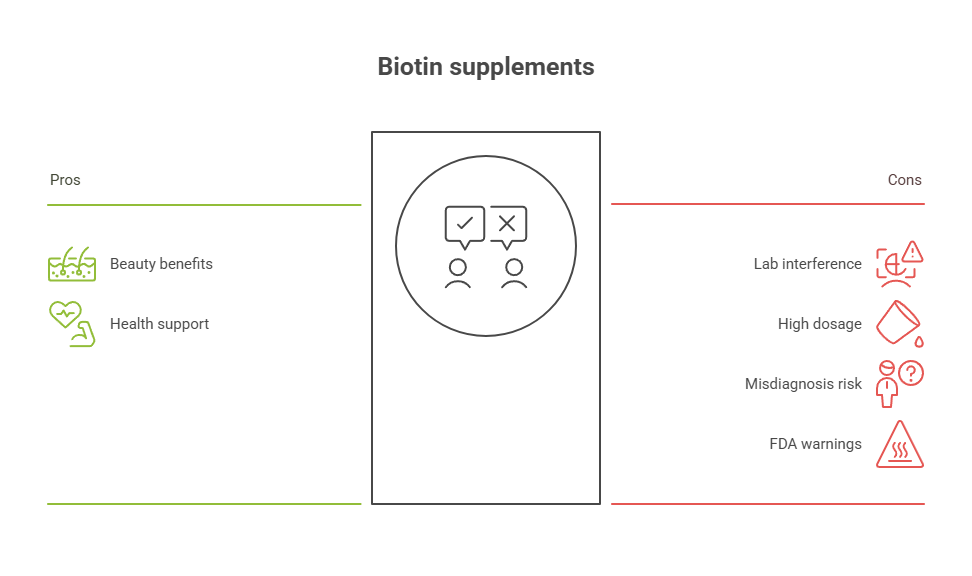
- The Popularity Explosion: Marketed relentlessly as the key to luscious hair, glowing skin, and strong nails, biotin is now a staple in “beauty” supplements and multivitamins. The problem is the dosage. While the daily requirement is only about 30 micrograms, these supplements often contain 5,000, 10,000, or even 20,000 micrograms—hundreds or thousands of times the necessary amount.
- The Analytical Catastrophe: As discussed, the highly sensitive biotin-streptavidin assay is the workhorse of modern labs. When a blood sample is saturated with supplemental biotin, it overwhelms the test.
- In “sandwich” assays, excess biotin prevents the test components from forming their proper “sandwich” structure, leading to a falsely low result. This affects:
- Troponin: The key marker for diagnosing a heart attack. A false negative can lead to a patient being sent home from the ER during a cardiac event.
- Thyroid Stimulating Hormone (TSH): The primary test for thyroid function. A falsely low TSH could miss a diagnosis of hypothyroidism or lead to a misdiagnosis of hyperthyroidism.
- Other Hormones: PSA (prostate cancer screening), hCG (pregnancy), FSH, LH.
- In “competitive” assays, the interference has the opposite effect, creating a falsely high result. This affects:
- Thyroid Hormones (T4, T3): A falsely high reading could lead a doctor to diagnose hyperthyroidism and prescribe dangerous anti-thyroid medications.
- Other Hormones: Cortisol, Testosterone.
- In “sandwich” assays, excess biotin prevents the test components from forming their proper “sandwich” structure, leading to a falsely low result. This affects:
- The Critical Takeaway: The FDA has issued multiple safety warnings about biotin interference. The consensus is clear: You must stop taking any supplement containing biotin for a minimum of 72 hours (3 days) before any blood test. Read your multivitamin label; it’s often a hidden ingredient.
Other Supplements of Major Concern
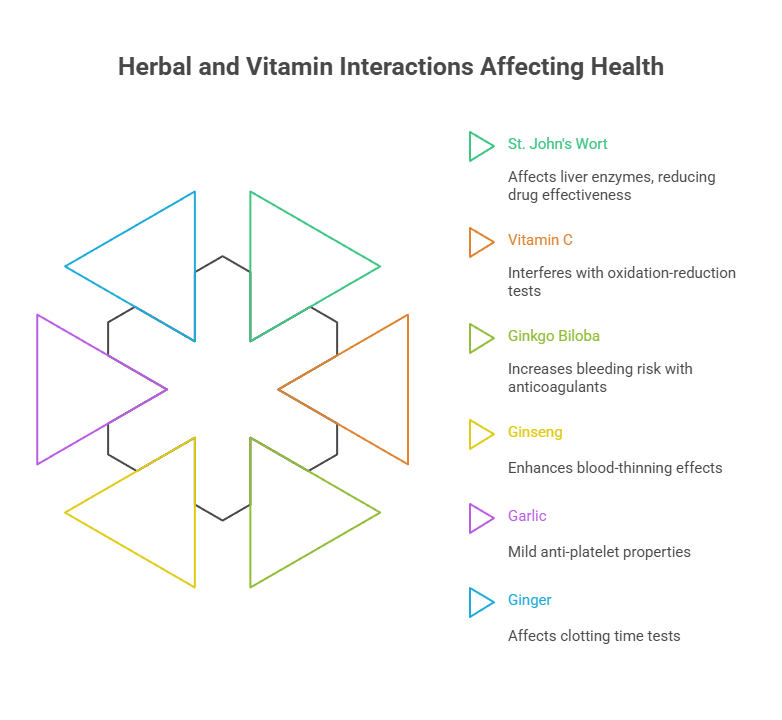
- St. John’s Wort: This popular herbal remedy for mood is notorious for its effect on the liver’s Cytochrome P450 enzyme system. In simple terms, it revs up the very enzymes your body uses to break down about 50% of all prescription drugs. This can cause the levels of critical medications like blood thinners, statins, and birth control pills to drop to ineffective levels. It is absolutely vital that your doctor and pharmacist know if you take this herb.
- Vitamin C (Ascorbic Acid): In high doses, Vitamin C is a strong antioxidant (a reducing agent). This chemical property can directly interfere with tests that use an oxidation-reduction reaction, leading to falsely low readings for glucose, creatinine, uric acid, and bilirubin.
- Ginkgo Biloba, Ginseng, Garlic, Ginger: Many popular herbs have mild anti-platelet or “blood-thinning” properties. When taken with prescription anticoagulants like warfarin or aspirin, they can increase the risk of bleeding. They can potentially affect clotting time tests.
The Over-the-Counter Minefield
Because they are so readily available, we often fail to consider OTC remedies as “real drugs.” This is a critical mistake.
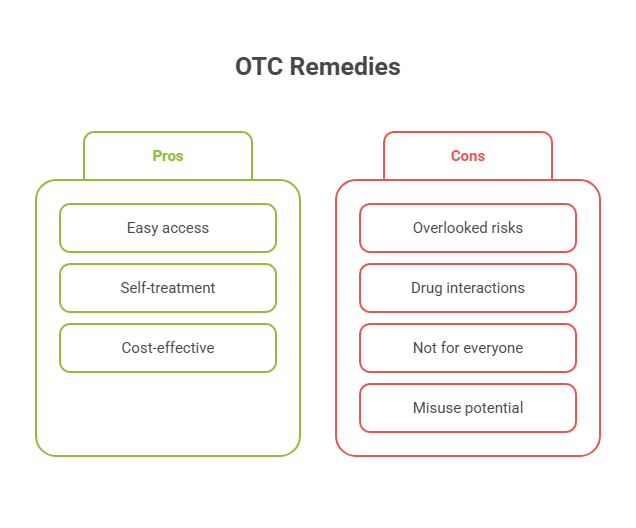
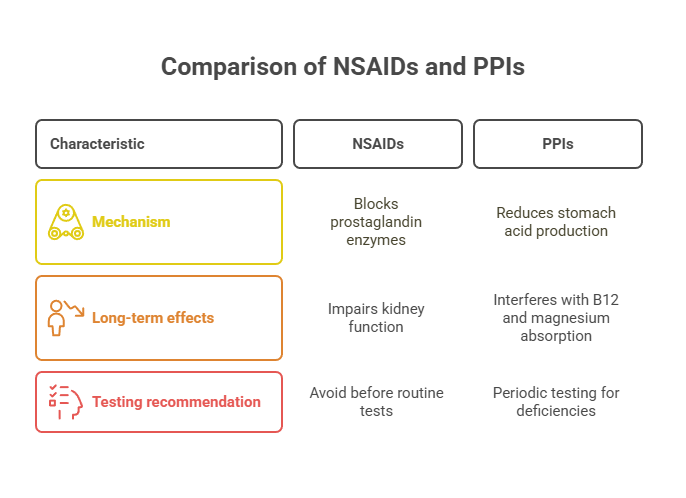
- NSAIDs (Ibuprofen, Naproxen): These work by blocking enzymes called prostaglandins. Some of these prostaglandins are protective for the stomach lining, while others help maintain blood flow to the kidneys. Chronic, heavy use of NSAIDs can impair kidney function, an effect that would be reflected in BUN and creatinine levels. For routine tests, it’s wise to ask your doctor if you should avoid them for 24-48 hours.
- Proton Pump Inhibitors (PPIs) (Omeprazole, Esomeprazole): These powerful stomach acid reducers are very effective, but long-term use (over a year) is strongly associated with interfering with the absorption of Vitamin B12 and magnesium. If you’re a chronic user, you should be periodically tested for deficiencies of these vital nutrients.
The Definitive Drug-Lab Test Interference Table
This table serves as a quick-glance reference. It is not exhaustive. Use it to inform your conversation with your doctor.
| Category | Substance / Drug Example | Common Brand Names | Key Tests Affected | Primary Mechanism | Recommended Action (Consult Doctor First) |
| Vitamins | Biotin (Vitamin B7) | Included in most Hair, Skin & Nails formulas | Thyroid (TSH, T3, T4), Troponin (Heart), Hormones (FSH, LH, Estradiol, Testosterone), PSA | Analytical: Directly interferes with common biotin-streptavidin lab assays. | CRITICAL: Stop for a minimum of 72 hours (3 days) before test. Inform doctor of dosage if you take it. |
| Vitamins | Vitamin C (Ascorbic Acid) | Various | Glucose, Uric Acid, Creatinine, Bilirubin, Fecal Occult Blood Test. | Analytical: Acts as a reducing agent, interfering with the chemical reactions in the test. | Inform doctor of high-dose use (>500mg/day). May need to pause before specific tests. |
| Vitamins | Vitamin B12 | Various | Long-term Metformin use can lower B12 levels. | Physiological: Metformin interferes with B12 absorption in the gut. | If on Metformin long-term, request a B12 level test periodically. |
| Herbal Supplements | St. John’s Wort | Perika, Kira | Liver Function (ALT, AST), Cyclosporine, Digoxin, Warfarin levels. | Physiological: Induces liver enzymes (Cytochrome P450), speeding up the metabolism of many drugs. | CRITICAL: Your doctor and pharmacist must know if you take this. It has numerous, serious drug interactions. |
| Herbal Supplements | Ginkgo Biloba, Ginseng | Various | Prothrombin Time (PT/INR), Platelet Function Tests. | Physiological: Can have anti-platelet (“blood-thinning”) effects. | Inform doctor, especially if you are on blood thinners or scheduled for surgery. |
| OTC Pain/Fever | NSAIDs (Ibuprofen, Naproxen) | Advil, Motrin, Aleve | Kidney Function (BUN, Creatinine), Liver Function (ALT, AST), Lithium levels. | Physiological: Can reduce blood flow to the kidneys; high doses can stress the liver. | For routine tests, ask if you should avoid for 24-48 hours. Do not stop if prescribed for a chronic condition. |
| OTC Stomach | Proton Pump Inhibitors (PPIs) | Prilosec, Nexium | Magnesium, Vitamin B12. | Physiological: Long-term use impairs absorption of these nutrients. | Discuss with doctor about testing for deficiencies if you are a long-term user. |
| Prescription: Cardio | Diuretics (e.g., HCTZ, Furosemide) | Lasix, Microzide | Electrolytes (Potassium, Sodium, Calcium), Kidney Function (BUN, Creatinine), Uric Acid. | Physiological: Primary function is to alter fluid and electrolyte balance. | DO NOT STOP. Your doctor is prescribing this to affect these levels and will monitor them. |
| Prescription: Cardio | Beta-Blockers (e.g., Metoprolol) | Lopressor, Toprol XL | Lipid Panel (can increase Triglycerides, lower HDL “good” cholesterol). | Physiological: Affects fat and glucose metabolism. | DO NOT STOP. This is a known effect that your doctor manages as part of your overall cardiac health. |
| Prescription: Endocrine | Corticosteroids (e.g., Prednisone) | Deltasone | Glucose, Lipid Panel (Cholesterol, Triglycerides), White Blood Cell Count. | Physiological: Has widespread effects on metabolism and the immune system. | DO NOT STOP. Effects are known and expected. Doctor will interpret results in this context. |
| Prescription: Endocrine | Thyroid Medication (Levothyroxine) | Synthroid, Levoxyl | TSH, Free T4. | Physiological: This is hormone replacement; it is intended to directly alter these levels. | DO NOT STOP. Ask your doctor if they prefer you take your pill before or after the blood draw for consistency. |
| Prescription: CNS | Antidepressants (e.g., SSRIs, Tricyclics) | Prozac, Zoloft, Amitriptyline | Can affect sodium levels (SIADH). Some can cause false positives on urine drug screens. | Physiological & Analytical: Can affect ADH secretion; structural similarity to drugs of abuse. | DO NOT STOP. Be aware of these potential effects and ensure your lab knows your medication list. |
FAQ – Your Top 11 Questions Answered
- What does “fasting” really mean for a blood test?
Fasting means consuming zero food or beverages for a designated period (typically 8-12 hours). The only exception is plain water. This absolutely means no coffee (not even black), no tea, no juice, no soda, no chewing gum, and no smoking. Coffee, for example, can stimulate the digestive system and transiently affect glucose levels. Water is highly encouraged because staying hydrated plumps up your veins, making the blood draw much easier. - I had a glass of wine last night. Do I need to reschedule my test?
For the most accurate results on a lipid panel (cholesterol and triglycerides) and a liver function test, it is best to avoid all alcohol for at least 24-48 hours. Alcohol can significantly and temporarily increase your triglyceride levels and can also cause a temporary spike in a liver enzyme called GGT. If the test is for something else, it may not matter as much, but honesty with the lab is the best policy. - Can topical medications like creams, gels, or patches affect blood tests?
Yes, absolutely, and this is a critically overlooked area. Topical hormone creams (testosterone, estrogen, progesterone) are a major source of contamination. If you apply a testosterone gel and then your partner has a blood test, you can transfer it to them via skin contact, causing bizarrely high levels in their results. Always apply these with gloves, wash hands thoroughly, and tell the phlebotomist which arm you use so they can draw from the opposite arm or another site. - Is it safe to take Tylenol (acetaminophen) before a blood test?
For most common blood tests, taking a standard, recommended dose of acetaminophen is very unlikely to cause interference. However, it’s important to know that an overdose of acetaminophen is a leading cause of acute liver failure, so it will dramatically affect liver function tests (ALT/AST) in that context. If you are a chronic user, your doctor should be aware. For a routine test, it is generally considered safe. - Help! I forgot and took a medication I was supposed to skip. What should I do?
Do not panic. Honesty is the only correct path. When you get to the lab, tell the phlebotomist exactly what you took and when you took it. They will note it on the requisition form. You should also call your doctor’s office to let them know. They will decide whether to proceed and interpret the results with that knowledge, or reschedule the test for a “clean” reading. - Does the timing of my daily medication matter on the day of the test?
For some drugs, yes. This is most important for drugs where the dose is titrated based on blood levels. The best example is levothyroxine (for thyroid). Taking the pill can cause a transient spike in T4 and a dip in TSH a few hours later. Many endocrinologists prefer you to consistently either take it before the test or wait until after. Ask your doctor what they prefer for your specific medication. - How do I talk to a doctor who seems to dismiss my supplement use?
This is a common and frustrating challenge. Frame the conversation around accuracy and partnership. Instead of just handing them a list, try saying: “I want to be a partner in making sure my lab results are as accurate as possible. I’ve read that some supplements, especially high-dose biotin, can seriously interfere with tests. Could we please review my list together to see if I should pause anything before my blood draw?” This approach is collaborative, not confrontational. - Can a single dose of a medication or supplement affect a test?
It depends on the substance and the test. A single dose of biotin can cause massive interference within hours. A single dose of an NSAID is unlikely to change your kidney function results unless you already have underlying disease. A single large dose of alcohol can absolutely skew your triglycerides. The rule of thumb is that if it’s a known interferent, it’s better to avoid it. - What about exercise? Can I work out before a blood test?
It is best to avoid strenuous or intense exercise for 24 hours before a blood test. Vigorous muscle activity can lead to a temporary increase in Creatine Kinase (CK), which could be mistaken for muscle damage from a statin or other condition. It can also slightly affect kidney function markers and lactate levels. A gentle walk is perfectly fine. - Can stress or a bad night’s sleep affect my lab results?
Yes, to a degree. Acute, severe stress (like a panic attack on the way to the lab) can temporarily raise levels of hormones like cortisol and adrenaline, and may slightly increase your white blood cell count. Chronic stress and poor sleep can contribute to inflammation, which might be reflected in markers like C-Reactive Protein (CRP). While you can’t always control it, it’s useful context for your doctor to have. - Do food-drug interactions, like grapefruit juice, matter for lab tests?
Indirectly, yes. Grapefruit juice is famous for inhibiting the same Cytochrome P450 enzymes in the gut that St. John’s Wort induces in the liver. By inhibiting these enzymes, it can cause the levels of certain drugs (like some statins and blood pressure meds) to rise to potentially toxic levels. A blood test would then accurately reflect this dangerously high drug level. This highlights how everything you consume can be part of the complex puzzle.
The Proactive Patient’s Toolkit – Your 4-Step Action Plan
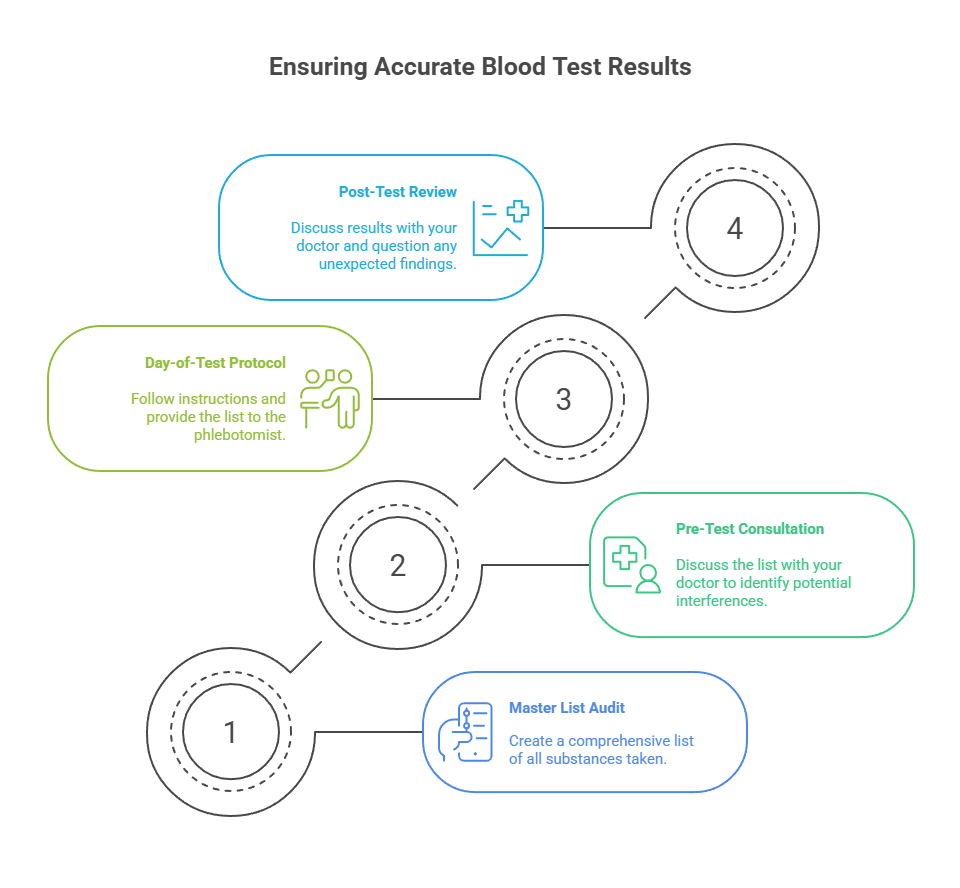
- Step 1: The Master List Audit (Do this today)
Go through your entire home and create a single, definitive list of every substance you take. Use a simple format: Substance Name, Dosage, and Frequency. Be exhaustive—prescriptions, vitamins, one-a-day herbs, protein powders, occasional pain relievers, everything. Keep this list on your phone or in your wallet. - Step 2: The Pre-Test Consultation (The Doctor Dialogue)
When a blood test is ordered, produce your Master List. Use this script: “Here is my complete list of medications and supplements. Since accuracy is so important, can you please tell me if I need to temporarily stop taking any of these before my test, and for how long?” Write down the specific instructions. - Step 3: The Day-of-Test Protocol (The Lab Visit)
Adhere to all fasting and medication instructions perfectly. Drink plenty of water. Bring your Master List with you. When you sit in the phlebotomist’s chair, provide the list to them as a final safety check. This simple act can prevent errors. - Step 4: The Post-Test Review (The Results Dialogue)
When discussing your results with your doctor, actively participate. If a result is unexpected, ask the critical question: “Is it possible that any of my medications or underlying conditions could be causing this result, or does it represent a new problem?”
From Patient to Partner
The intricate dance between the substances we take and the tests we undergo is not a reason for fear, but a call for empowerment. It is a powerful reminder that you are not merely a passive recipient of healthcare, but the central, most vital member of your own medical team. Your body’s health data is one of your most precious assets. By embracing the role of a diligent, communicative, and informed partner, you elevate the quality of your care. You ensure that the critical decisions being made about your health are based not on a distorted snapshot, but on the truest, most accurate reflection of your well-being.

