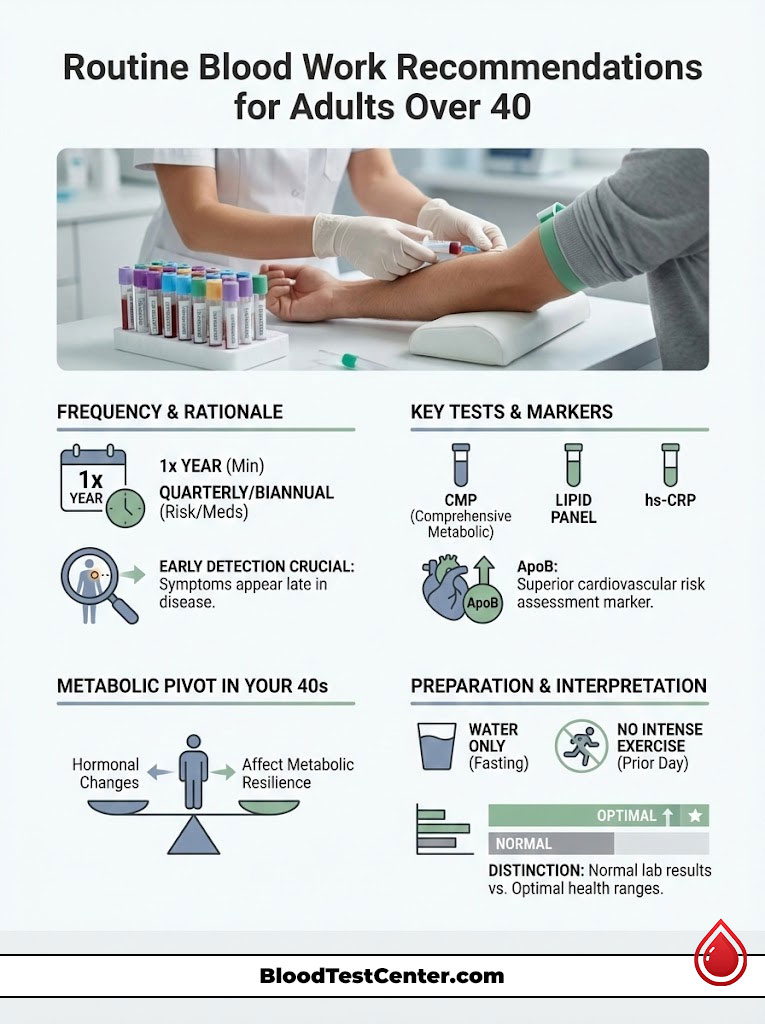
You turn 40, and the biological rules of engagement change. In my 15 years as a Board-Certified Internist, I have observed a distinct, undeniable shift in patient physiology the moment they enter their fourth decade. The body becomes significantly less forgiving of dietary errors, recovery times from exercise lengthen, and silent metabolic risks begin to accumulate in the background. For many, this is the “Metabolic Pivot.” It is the critical decade where prevention must transition from a passive idea to an active, data-driven strategy.
Table of Contents
The question I hear most frequently in the clinic is: How often should adults over 40 get routine blood work? The standard answer from insurance companies and general guidelines is often “once a year,” but optimal health requires a much more nuanced approach. While annual screening is the absolute baseline, the ideal frequency depends heavily on your specific risk profile, your family history, and your aggressive metabolic goals. Treating blood work as a strategic tool rather than a mandatory chore is the single most effective way to detect chronic disease before it becomes irreversible.

Quick Answer: The Ideal Frequency
How often should adults over 40 get routine blood work? Generally, healthy adults should schedule comprehensive labs annually. However, if you have borderline markers (such as prediabetes or elevated cholesterol), a family history of heart disease, or are adjusting medications, the frequency should increase to every 3 to 6 months. This tighter interval allows for rapid course correction before minor imbalances become chronic conditions.
Determining Frequency: One Size Does Not Fit All
In medicine, we distinguish between the “Standard of Care” and “Optimal Care.” Standard of Care usually refers to the minimum requirements set by national guidelines to prevent immediate catastrophe or death. Optimal Care, however, focuses on longevity, vitality, and performance. When determining how often should adults over 40 get routine blood work, we must look far beyond the minimums.
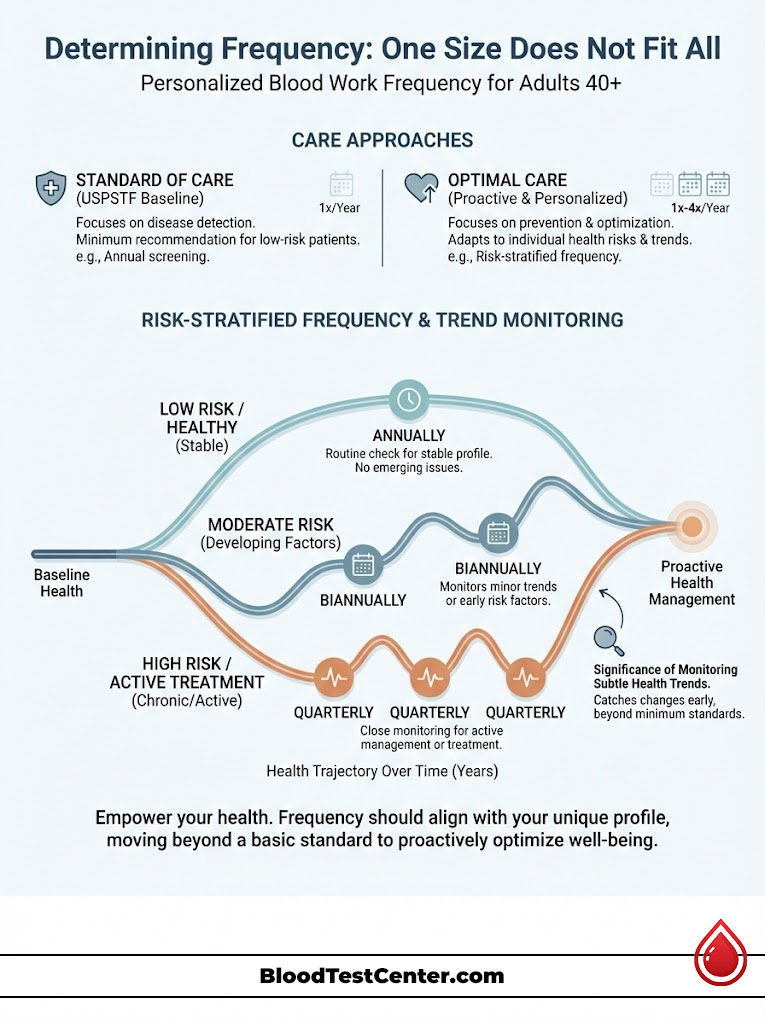
The U.S. Preventive Services Task Force (USPSTF) provides Grade A and B recommendations that influence insurance coverage. For a generally healthy 40-year-old, these guidelines support an annual physical. Yet, in practice, a year is a remarkably long time in metabolic terms. A lot can happen to your vascular system, your insulin sensitivity, and your hormone levels in 12 months.
The Baseline Recommendation
For patients with absolutely no symptoms, a normal body weight (BMI 18.5-24.9), and a clean family history, routine blood work once a year is sufficient. This annual look “under the hood” establishes a baseline. We compare this year’s data against last year’s to spot trends. Is your glucose creeping up by a few points? Is your kidney function drifting down? These subtle shifts are invisible without consistent annual data points.
Risk-Stratified Frequency
The schedule changes immediately if risk factors represent a concern. Here is how I stratify frequency in my private practice to ensure nothing slips through the cracks:
- The 3-Month Interval: This is for active management. If we start a patient on a statin for high cholesterol, hormone replacement therapy, or Metformin for blood sugar, we cannot wait a year to see if it works. We re-test in 12 weeks. This is also the necessary cycle for patients actively trying to reverse metabolic syndrome through diet and exercise.
- The 6-Month Interval: This targets the “borderline” patient. Perhaps your HbA1c is 5.7% (pre-diabetic range) or your blood pressure is slightly elevated. You do not need quarterly draws, but waiting a year risks letting the condition progress to full-blown disease. A six-month check-in keeps you accountable and provides a safety net.
Key Statistics: The 40s Risk Profile
- 40% of U.S. adults aged 40–59 have obesity, a primary driver of metabolic disease (CDC).
- 1 in 3 adults have prediabetes, and more than 80% do not know they have it.
- Cardiovascular risk scores (ASCVD) begin to rise significantly after age 40.
- Thyroid dysfunction affects women 5 to 8 times more frequently than men, often appearing during perimenopause.
- Testosterone levels in men drop by approximately 1% per year after age 30, accelerating in the 40s.
Comparison Table: Blood Work Frequency by Risk Profile
| Patient Profile | Recommended Frequency | Key Focus Areas | Clinical Reasoning |
|---|---|---|---|
| Low Risk / Healthy | Annually (Every 12 Months) | Lipid Panel, CMP, CBC, A1c | Establish baselines; screen for silent onset of disease. |
| Moderate Risk | Biannually (Every 6 Months) | Targeted markers (e.g., Glucose, Lipids) | Monitor “borderline” metrics like HbA1c 5.7-6.0% or elevated LDL. |
| High Risk / Active Treatment | Quarterly (Every 3 Months) | Liver function, Kidney function, Drug levels | Assess efficacy of new medications or aggressive lifestyle interventions. |
The Physiology of the 40s: Why Frequency Changes Now
Why is the question of how often should adults over 40 get routine blood work so vital right now? The answer lies in physiology. Your body at 40 is fundamentally different from your body at 30. The mechanisms of repair begin to slow down, and the mechanisms of decay begin to speed up.
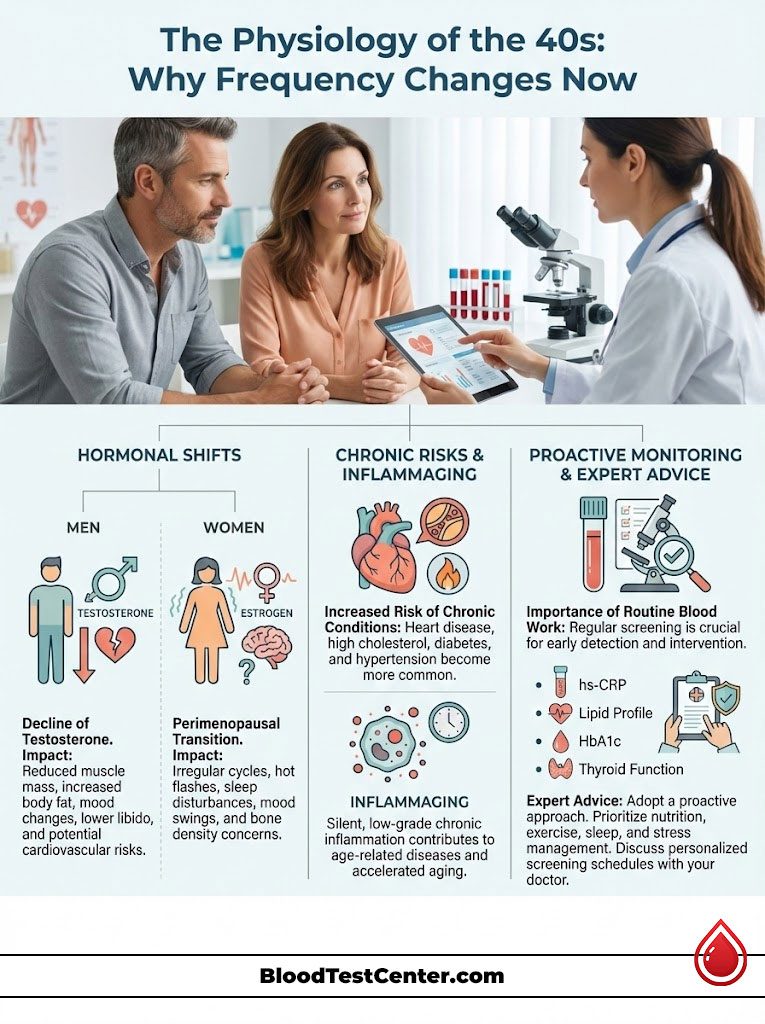
Hormonal Shifts and Metabolic Slowdown
For men, testosterone levels decline gradually. This is often referred to as “andropause.” It affects muscle mass, bone density, and most critically, insulin sensitivity. Lower testosterone is directly linked to an increase in visceral fat—the dangerous belly fat that wraps around organs.
For women, the 40s mark the perimenopausal transition. This is a time of extreme hormonal volatility. Estrogen is cardioprotective; it keeps arteries flexible and helps manage cholesterol. As estrogen levels fluctuate and eventually drop, women often experience sudden spikes in LDL cholesterol and blood pressure that were previously well-controlled. Routine blood work captures these hormonal consequences before they manifest as a heart attack or stroke.
The Concept of “Inflammaging”
Aging is associated with a chronic, low-grade inflammation known in the medical community as “inflammaging.” This systemic inflammation damages blood vessels, joints, and brain tissue. Unlike acute inflammation (like a sprained ankle or a bee sting), you cannot feel this. It is silent and insidious.
By increasing the frequency of routine blood work, we can monitor inflammatory markers like hs-CRP (High-Sensitivity C-Reactive Protein). This gives us a chance to intervene with anti-inflammatory nutrition, targeted supplementation, or stress management protocols before the damage becomes permanent.
Expert Insight
“In my practice, I tell patients that their 40s are the ‘decade of verification.’ You can no longer assume you are healthy just because you feel okay. High blood pressure and high cholesterol are asymptomatic until they cause a catastrophic event. Blood work provides the feedback loop necessary to correct course.”
The Essential “Big Five” Lab Panels
When you schedule your routine blood work, specific panels provide the highest yield of actionable data. We call these the “Big Five.” If your doctor does not order these, you should request them specifically.
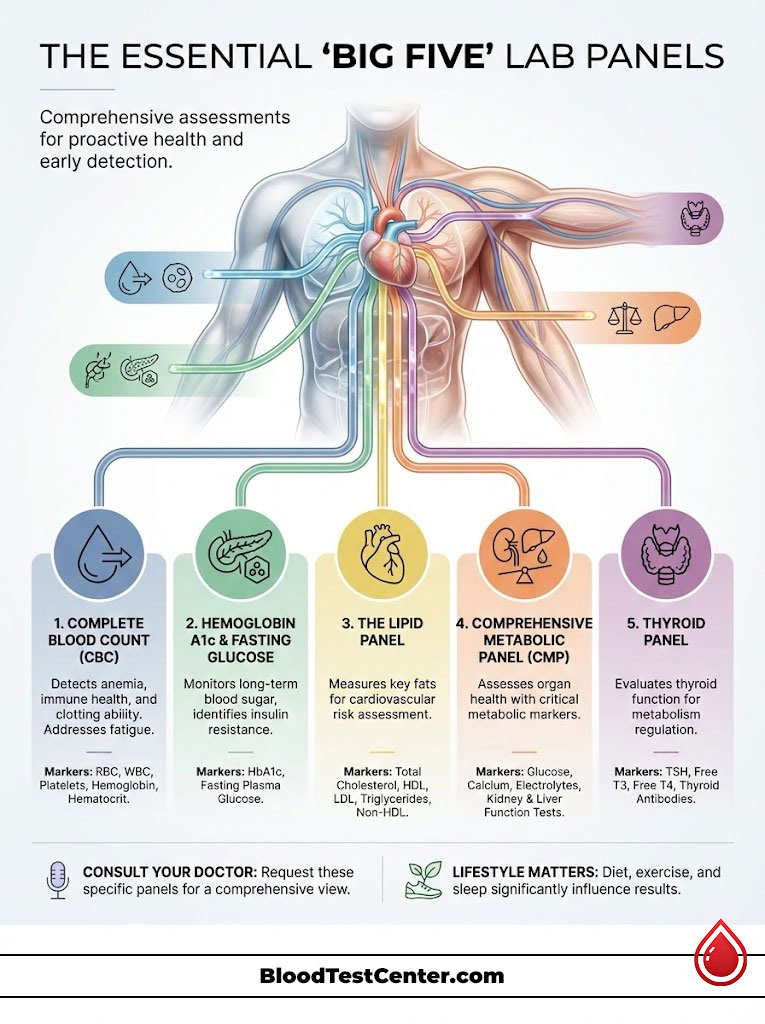
1. The Lipid Panel (Cardiovascular Risk Profile)
Heart disease remains the leading killer in the USA. A standard lipid panel measures Total Cholesterol, HDL (good), LDL (bad), and Triglycerides. However, for adults over 40, we need to look deeper than these basic numbers.
We pay close attention to Non-HDL cholesterol. This number aggregates all the “bad” cholesterol particles that contribute to plaque buildup. According to the American Heart Association (AHA), keeping Non-HDL low is a primary target for prevention. Furthermore, Triglycerides are a direct reflection of your carbohydrate intake and insulin sensitivity. If your Triglycerides are high (above 100 mg/dL), it is often a dietary red flag indicating too much sugar or alcohol.
2. Hemoglobin A1c (HbA1c) & Fasting Glucose
With the prediabetes epidemic exploding, monitoring blood sugar is non-negotiable. Hemoglobin A1c gives us a three-month average of your blood sugar levels. Unlike a simple fasting glucose test, which can vary based on what you ate for dinner last night or how well you slept, A1c tells the truth about your long-term habits. A result above 5.7% signals insulin resistance, a condition that drives aging, weight gain, and vascular damage.
3. Comprehensive Metabolic Panel (CMP)
The Comprehensive Metabolic Panel (CMP) is a broad sweep of your organ health. It includes several critical markers:
- Liver Function (ALT/AST): Non-Alcoholic Fatty Liver Disease (NAFLD) is rising rapidly in the 40+ demographic, often driven by visceral fat and fructose consumption.
- Kidney Function (eGFR/Creatinine): Filtration rates naturally decline with age. We monitor this to ensure medications or high-protein diets aren’t stressing the kidneys.
- Electrolytes: Sodium, potassium, and calcium levels help us manage blood pressure, hydration status, and heart rhythm health.
4. Complete Blood Count (CBC)
Fatigue is a common complaint in the 40s, but it shouldn’t be dismissed as “just aging.” A Complete Blood Count checks for hidden anemia (low red blood cells or iron), which is a common cause of exhaustion. It also looks at white blood cells, which serve as markers for immune health and chronic infection. Platelet counts are also checked to assess clotting ability, which is vital as stroke risk increases.
5. Thyroid Panel (TSH, T3, T4)
The thyroid is the master regulator of metabolism. If your thyroid is sluggish, you will gain weight, feel tired, lose hair, and experience brain fog regardless of how much you exercise. Standard routine blood work often only checks TSH (Thyroid Stimulating Hormone).
However, for adults over 40, specifically women, I advocate for a full panel including Free T3, Free T4, and Thyroid Antibodies. This helps rule out Hashimoto’s thyroiditis or subclinical hypothyroidism—a state where labs are “normal” according to the lab sheet, but symptoms persist and metabolism suffers.
Advanced Biomarkers: Moving from Normal to Optimal
To truly answer how often should adults over 40 get routine blood work effectively, we must look at advanced markers. These go beyond the basic physical and offer a high-definition view of your health. These are the tests that longevity experts rely on.

High-Sensitivity C-Reactive Protein (hs-CRP)
This is the definitive marker for arterial inflammation. A high hs-CRP indicates that your blood vessels are inflamed, making plaque rupture more likely. It transforms the cardiovascular risk profile from a guess into a calculated assessment. If this is elevated, we look immediately at gut health, gum disease, or chronic stress.
ApoB (Apolipoprotein B)
Many lipidologists now prefer ApoB over LDL-C. ApoB measures the actual number of atherogenic particles in your blood, not just the concentration of cholesterol within them. It is a far more precise predictor of heart attack risk. If you have a family history of heart disease, demanding an ApoB test is essential.
Vitamin D (25-Hydroxy)
Vitamin D is actually a pro-hormone essential for immune function, mood regulation, and bone density. Osteopenia (pre-osteoporosis) can begin in the 40s. Checking Vitamin D levels ensures we can supplement correctly to protect your skeleton. Most adults in northern climates are chronically deficient.
Homocysteine
Elevated homocysteine is a risk factor for stroke, dementia, and heart disease. It often indicates a need for methylated B-vitamins (B12 and Folate). This is a simple fix that yields profound long-term protection, yet it is rarely checked in standard physicals.
Fasting Insulin
While A1c tells us your average blood sugar, Fasting Insulin tells us how hard your pancreas is working to keep that sugar down. High fasting insulin is the earliest warning sign of metabolic dysfunction, often appearing years before blood sugar rises. It is a critical marker for weight loss resistance in the 40s.
Interpreting Your Results: The “Normal” vs. “Optimal” Debate
When you receive your routine blood work results, you will see a “Reference Range.” It is vital to understand that these ranges are based on population averages—and the average American population is not metabolically healthy. The average American is overweight and pre-diabetic.
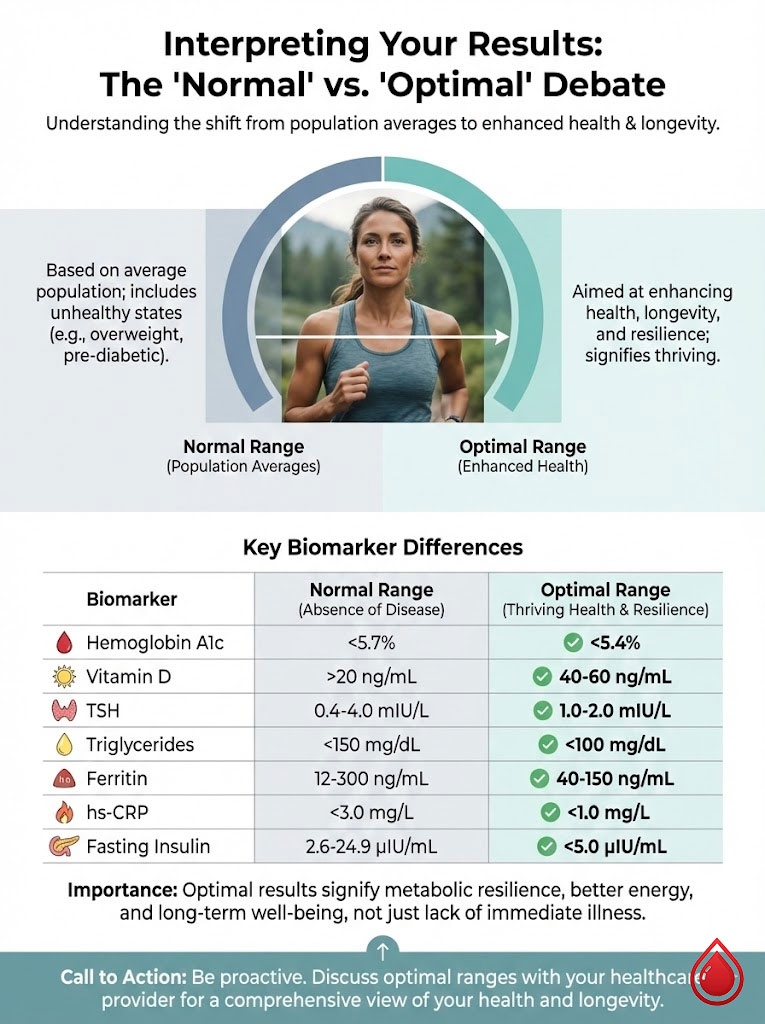
From a functional medicine and longevity perspective, we aim for “Optimal Ranges.” Being in the middle of the bell curve of a sick population is not the goal; being in the top percentile of health is. A “normal” result simply means you do not have a clinically diagnoseable disease yet. Optimal results mean you are resilient and thriving.
Comparison Table: Reference Ranges vs. Optimal Longevity Ranges
| Biomarker | Standard Reference Range | Optimal Longevity Range |
|---|---|---|
| Hemoglobin A1c | Below 5.7% | 4.8% – 5.2% |
| Vitamin D | 20 – 50 ng/mL | 50 – 80 ng/mL |
| TSH (Thyroid) | 0.4 – 4.5 mIU/L | 1.0 – 2.0 mIU/L |
| Triglycerides | Below 150 mg/dL | Below 80 mg/dL |
| Ferritin (Iron) | 30 – 400 ng/mL | 50 – 100 ng/mL |
| hs-CRP (Inflammation) | Below 3.0 mg/L | Below 1.0 mg/L |
| Fasting Insulin | 2.6 – 24.9 uIU/mL | 2.0 – 5.0 uIU/mL |
Logistics: Preparing for Your Blood Draw
The accuracy of your routine blood work depends heavily on your preparation. Poor preparation can lead to false positives, skewed data, and unnecessary anxiety.
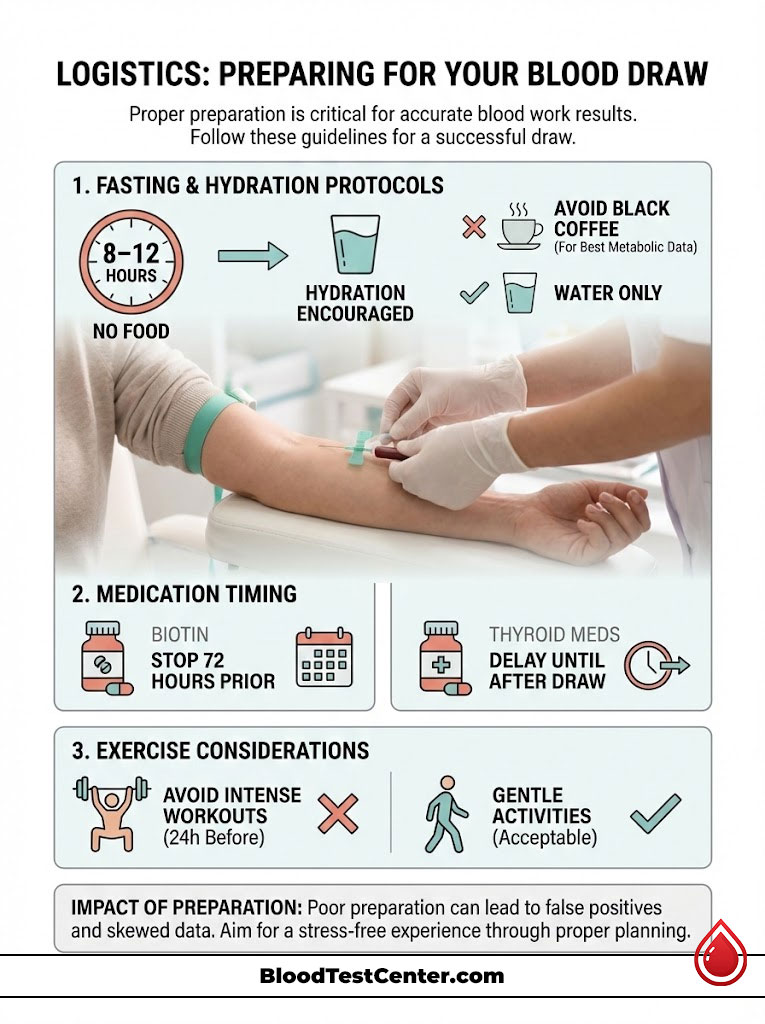
Fasting Protocols
Fasting for blood work is standard for glucose and lipid panels. The general rule is 8 to 12 hours of no food. Water is encouraged; in fact, being well-hydrated makes the phlebotomist’s job easier and the draw less painful. Dehydration can artificially elevate hematocrit and electrolyte levels.
A common question is about coffee. Black coffee can slightly elevate cortisol and glucose due to caffeine stimulation. For the most accurate metabolic data, stick to water only on the morning of the test.
Medication and Supplement Timing
Supplements can interfere with lab assays. For example, Biotin (often found in hair, skin, and nail formulas) can cause false readings on thyroid tests and troponin (heart) tests. It is recommended to stop Biotin 72 hours before your draw. If you take thyroid medication, delay your morning dose until after the blood draw, as it can cause a temporary spike in T4 levels.
Exercise Considerations
Regarding exercise, avoid intense HIIT workouts or heavy weightlifting for 24 hours before a kidney function test or liver panel. Intense muscle breakdown releases creatinine and liver enzymes, which can falsely signal organ distress on a Comprehensive Metabolic Panel. A gentle walk is fine, but save the marathon training for after the appointment.
Insurance, Cost, and Access in the USA
Understanding the financial landscape is part of the process. Under the Affordable Care Act (ACA), most insurance plans are required to cover preventive screening at 100% (no copay) once per year. This usually includes a lipid panel and glucose check.

However, diagnostic codes matter immensely. If your doctor codes the labs as “Screening” (Code Z00.00), it is often covered. If they code it for a specific symptom like “Fatigue” or “Brain Fog,” it becomes diagnostic. Diagnostic tests usually apply to your deductible, meaning you might pay out of pocket until that deductible is met.
Routine blood work generally falls under preventive care, but advanced markers like ApoB, Insulin, or comprehensive hormone panels may not be covered by basic plans. Direct-to-consumer testing has risen as a solution for those who want more frequent data. Services like Quest and LabCorp now allow patients to order their own labs out-of-pocket, providing autonomy for those who want to track their health quarterly without insurance hurdles.
Actionable Steps After Results
Getting the blood drawn is only step one. The value lies in the interpretation and the subsequent action plan.
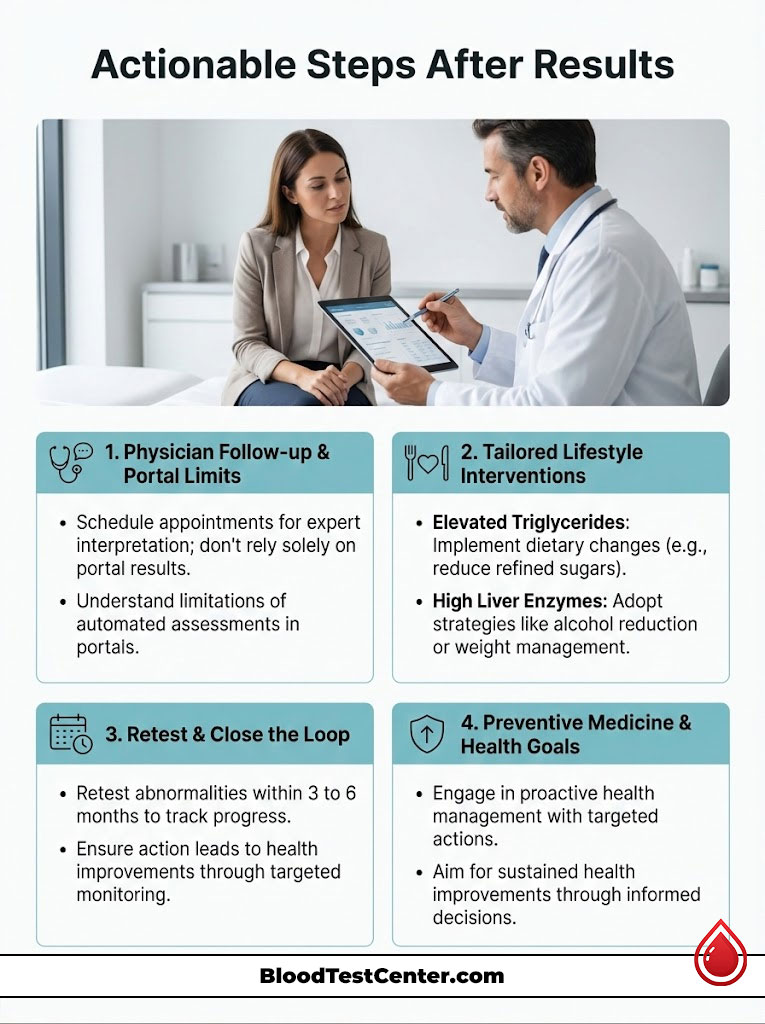
The Follow-Up Appointment: Never rely on a patient portal to tell you if you are healthy. Always review results with a physician who understands your history. A “normal” flag on a portal does not account for the nuance of your personal risk factors or family history.
Lifestyle Interventions: If your Lipid panel shows elevated triglycerides, the immediate move is to reduce simple carbohydrates and alcohol. If your liver enzymes are high, we look at visceral fat reduction and toxin exposure. We use the data to create a targeted plan, not a generic one.
Retesting Timeline: If we find an abnormality, we do not wait a year. We retest that specific marker in 3 to 6 months to verify that our interventions are working. This closes the loop on preventive medicine and ensures you are actually getting healthier, not just hoping for the best.
The Role of Wearable Tech in Monitoring
While routine blood work provides a snapshot in time, modern wearable technology offers a continuous movie of your health. Devices that track heart rate variability (HRV), resting heart rate, and sleep quality can serve as early warning systems between blood draws.

For example, a sudden, sustained drop in HRV or a rise in resting heart rate can indicate systemic stress or illness weeks before you feel it. When combined with annual or biannual blood work, these devices create a comprehensive safety net. However, they do not replace the need for biochemical analysis; they simply complement it.
Summary & Key Takeaways
So, how often should adults over 40 get routine blood work? The answer is a minimum of once per year, but quarterly or biannually if you are actively managing risks, taking medication, or optimizing for longevity. Your 40s represent a critical window where the body is still responsive to change, but the risks of inaction rise steeply.
Routine blood work is the dashboard of the human body. It provides the objective data required to navigate the aging process with confidence. Do not wait for symptoms to appear. Symptoms are often the last stage of a disease process, not the first.
If you have not had a Comprehensive Metabolic Panel or Lipid panel in the last 12 months, consider this your call to action. Schedule your physical, request the “Big Five” panels, and take ownership of your metabolic future. Your future self will thank you for the diligence you apply today.
Frequently Asked Questions
How often should a healthy adult over 40 schedule routine blood work?
For adults with no symptoms and a low-risk profile, I recommend a comprehensive blood panel at least once every 12 months. This annual frequency allows us to establish a metabolic baseline and monitor subtle year-over-year shifts in kidney function, glucose regulation, and lipid profiles before they manifest as chronic disease.
Why should I get blood work every three to six months if I have borderline markers?
If you are in the “borderline” range for markers like HbA1c or LDL cholesterol, waiting a full year to retest is risky because metabolic damage can accelerate quickly in your 40s. A tighter 3-to-6-month interval provides a necessary feedback loop to verify if lifestyle interventions or medications are successfully moving your biomarkers back into the optimal range.
What is the Metabolic Pivot and why does it matter for my lab results?
The Metabolic Pivot refers to the physiological shift in your 40s where hormonal declines, such as dropping testosterone or perimenopausal estrogen fluctuations, reduce your metabolic resilience. During this decade, your body becomes less efficient at processing glucose and managing inflammation, making frequent biochemical monitoring essential for early intervention.
Why is ApoB considered a superior marker to standard LDL cholesterol for heart health?
While a standard lipid panel measures the concentration of cholesterol, ApoB measures the actual number of atherogenic particles that cause plaque buildup in your arteries. For patients over 40, ApoB provides a far more precise assessment of cardiovascular risk, especially if you have a family history of heart disease or metabolic syndrome.
Can I drink black coffee before my fasting blood draw?
I advise my patients to stick to plain water only during the 8-to-12-hour fasting window. While black coffee has no calories, the caffeine can stimulate a release of cortisol and glucose from the liver, which may slightly skew your fasting insulin and blood sugar results.
How does intense exercise the day before a blood test affect my results?
Heavy weightlifting or high-intensity interval training (HIIT) within 24 hours of a blood draw can cause temporary spikes in liver enzymes (AST/ALT) and creatinine levels due to muscle breakdown. To ensure your Comprehensive Metabolic Panel (CMP) accurately reflects your organ function, avoid strenuous workouts the day before your appointment.
What is the difference between a normal lab result and an optimal longevity range?
Standard “normal” ranges are based on population averages that include many unhealthy individuals, whereas “optimal” ranges are targeted toward peak performance and disease prevention. For instance, while a TSH of 4.0 may be “normal” on a lab report, an optimal range for vitality and metabolic health is typically between 1.0 and 2.0 mIU/L.
Why is it important to test high-sensitivity C-reactive protein (hs-CRP) after age 40?
The hs-CRP test measures systemic inflammation, often referred to as “inflammaging,” which is a primary driver of arterial damage and cognitive decline. Monitoring this marker allows us to identify “silent” inflammation that doesn’t cause pain but significantly increases your risk for a catastrophic cardiovascular event.
Should I stop taking Biotin supplements before my routine blood work?
Yes, you should discontinue Biotin (Vitamin B7) at least 72 hours before your blood draw. Biotin is known to interfere with the laboratory assays used to measure thyroid hormones and cardiac troponin, which can lead to dangerously inaccurate clinical interpretations.
Why is a full thyroid panel better than just a TSH test for women in their 40s?
TSH only measures the signal from the brain to the thyroid, but a full panel including Free T3, Free T4, and Thyroid Antibodies provides a complete picture of how the thyroid is actually functioning. In the 40s, women are at higher risk for subclinical hypothyroidism or Hashimoto’s, which a TSH-only screen often misses.
How does fasting insulin differ from Hemoglobin A1c in detecting metabolic issues?
Hemoglobin A1c measures your average blood sugar over three months, but fasting insulin can identify metabolic dysfunction years before your blood sugar actually rises. High fasting insulin tells us that your pancreas is overworking to maintain “normal” glucose levels, signaling early-stage insulin resistance that requires immediate lifestyle changes.
Will my insurance cover advanced biomarkers like ApoB or Vitamin D?
Most insurance plans cover basic preventive screenings like lipid panels and glucose at 100% once per year. However, advanced markers like ApoB or fasting insulin may require a specific diagnostic code related to symptoms or family history to be covered, so it is important to discuss clinical coding with your physician.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always consult with a Board-Certified physician or qualified healthcare professional before making health decisions, starting a new supplement regimen, or interpreting laboratory results.
References
- Centers for Disease Control and Prevention (CDC) – National Diabetes Statistics Report – Data on prediabetes prevalence and metabolic health in U.S. adults.
- U.S. Preventive Services Task Force (USPSTF) – A and B Recommendations – Official clinical guidelines for annual physicals and screening frequencies.
- American Heart Association (AHA) – Circulation Journal – Research regarding Non-HDL cholesterol and ApoB as superior predictors of cardiovascular risk.
- The Lancet Healthy Longevity – Inflammaging Research – Scientific breakdown of chronic low-grade inflammation and its role in the aging process.
- American Thyroid Association (ATA) – Thyroid Function Guidelines – Clinical standards for TSH, T3, and T4 testing in perimenopausal women.
- Journal of Clinical Endocrinology & Metabolism – Testosterone and Aging – Study on the annual decline of androgen levels in men over 30 and its metabolic impact.

