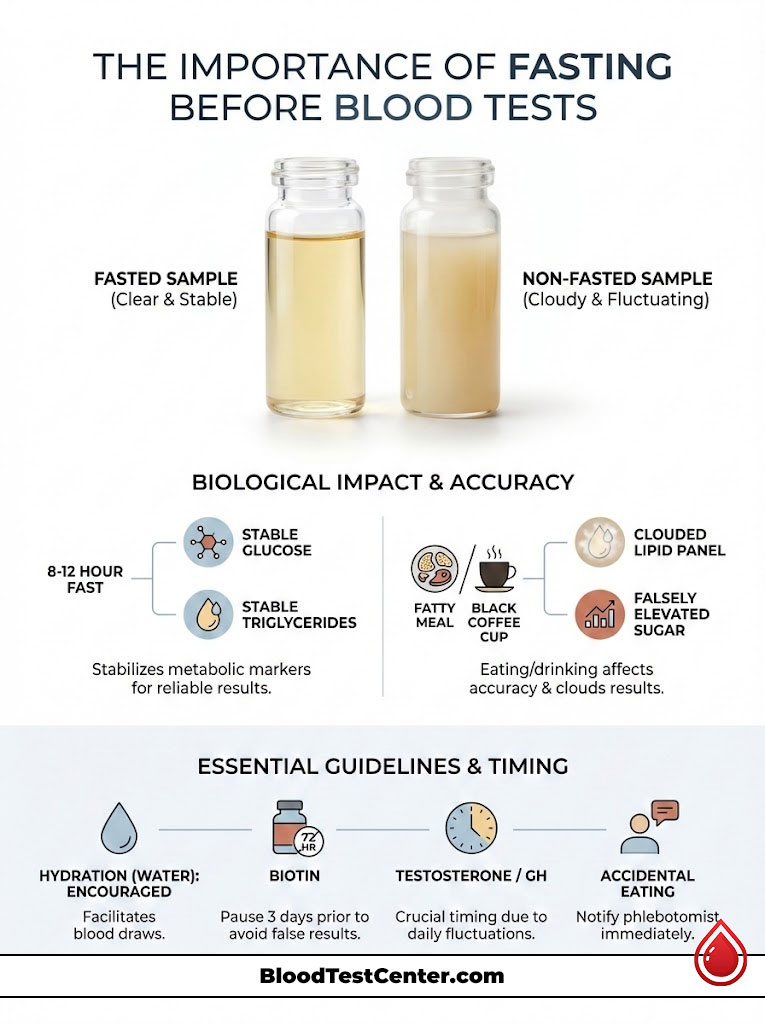
Yes, for specific diagnostic panels, fasting is a chemical necessity rather than a mere suggestion. While modern medical guidelines allow non-fasting samples for some initial screenings, tests like the Lipid Panel, Glucose, and Comprehensive Metabolic Panel (CMP) typically require an 8–12 hour fast. This period allows your body to clear dietary fats and stabilize blood sugar levels. Is it necessary to fast before a routine blood test? If your doctor orders these specific metabolic markers, the answer is a definitive yes to prevent misdiagnosis and ensure accuracy.
Table of Contents
It is 7:00 AM on a Tuesday. A patient sits in the phlebotomy chair with their sleeves rolled up. They are ready for their annual physical blood work. The phlebotomist asks the standard question regarding food intake. The patient smiles and admits to having a cup of black coffee. They assume it acts just like water.
As a clinical pathologist, I see this scenario play out in laboratories daily. That single cup of coffee often forces us to cancel the draw. It risks generating results that could lead to a false diagnosis of pre-diabetes or adrenal issues. The question—is it necessary to fast before a routine blood test—is one of the most critical inquiries in modern preventative medicine. The answer lies not in arbitrary rules. It lies in the complex biochemistry of your blood.
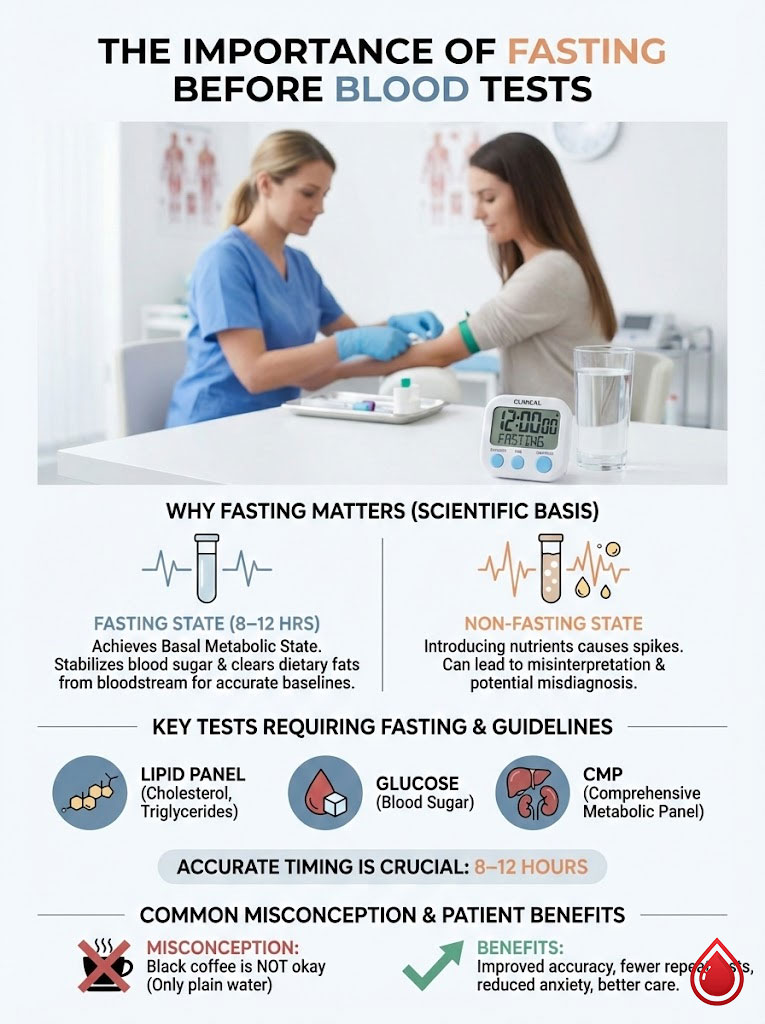
We are not asking you to starve yourself to be difficult. We are asking you to reach a basal state. This is a specific metabolic window. It is usually achieved after 8 to 12 hours of fasting. During this time, your body’s analytes are stable. They are not fluctuating wildly due to active digestion. Understanding this distinction can save you from repeat visits. It prevents unnecessary medication. It reduces medical anxiety.
Key Statistics & Data
- 12 Hours: The time required to fully clear dietary fat particles called chylomicrons from the bloodstream.
- 50% Increase: Triglycerides can rise by this amount within 2 hours of a standard meal.
- 72 Hours: How long you should pause high-dose Biotin supplements before a blood draw to avoid interference.
- 10-15%: The potential false elevation in glucose levels caused by caffeine intake prior to a test.
- 70-100 mg/dL: The standard reference range for fasting blood glucose. Eating can spike this well over 140 mg/dL instantly.
- 30 Minutes: The time it takes for insulin levels to spike after consuming simple carbohydrates.
The Physiology of Interference: Why Food Ruins Lab Data
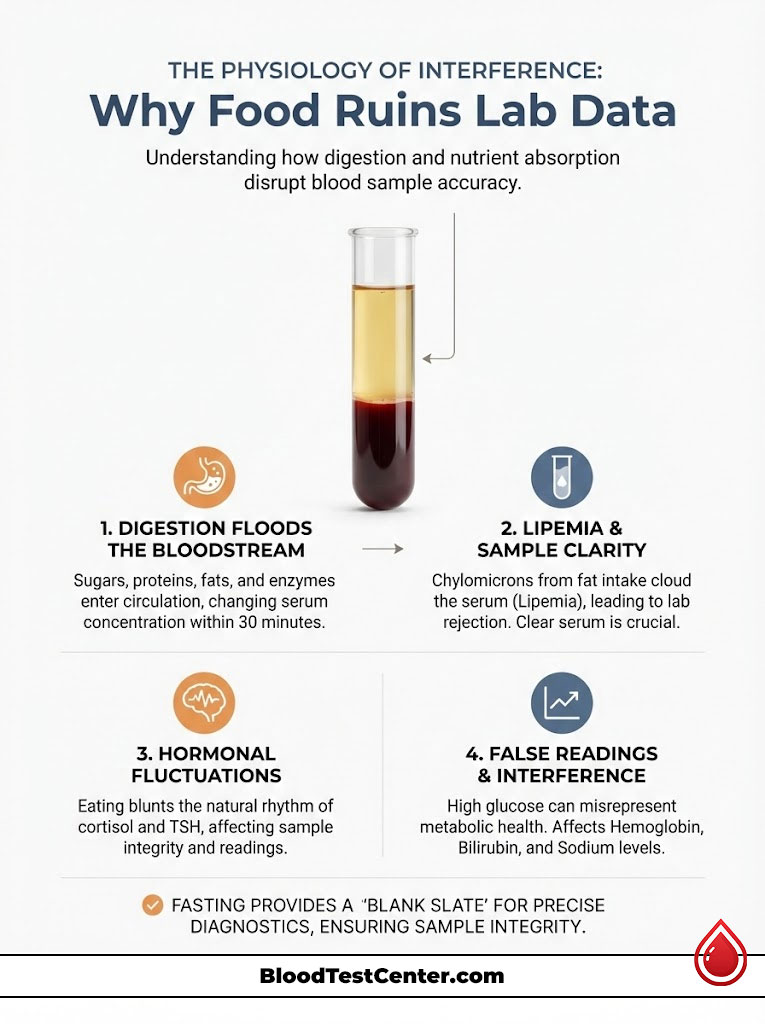
To understand why we request fasting, you must look at what happens inside your veins. Digestion is a violent chemical event. It floods the bloodstream with sugars, proteins, fats, and enzymes. This changes the composition of the sample we draw.
When you ask is it necessary to fast before a routine blood test, you are asking if we can filter out that noise. In many cases, we cannot. The interference happens on a microscopic level.
The Biochemistry of Eating
Your serum concentration changes within 30 minutes of eating. The most immediate shift is glucose homeostasis. Carbohydrates break down into glucose. This triggers your pancreas to release insulin. This hormone floods your system to manage the sugar.
We might draw your blood during this spike. Your glucose reading will be high. Your potassium levels may shift as insulin pushes potassium into your cells. This creates a false picture of your metabolic health. It mimics pathology where there is none.
Lipemia: The “Cloudy” Sample
This is the most visible issue in the laboratory. When you eat fat, your body produces chylomicrons. These are microscopic fat particles that transport lipids. Even a small amount of creamer can cause this.
In a fasting sample, the serum is a clear, golden-yellow fluid. In a non-fasting patient, chylomicrons turn that serum milky and white. We call this Lipemia. It is a major cause of sample rejection.
Pathologist’s Insight:
Why does milky serum matter? Modern lab analyzers use spectrophotometry. They shine a beam of light through the sample to measure chemicals. If your serum is cloudy from fat, the light cannot pass through. This causes error codes. It creates inaccurate readings for Hemoglobin, Bilirubin, and Sodium. We often have to reject these samples entirely.
Hormonal Fluctuations
Food intake resets your body’s hormonal clock. Cortisol is your stress hormone. It naturally peaks in the morning and drops at night. Eating can blunt or spike this rhythm.
Thyroid Stimulating Hormone (TSH) can also fluctuate based on caloric intake. We are often trying to diagnose a subtle hormonal imbalance. The noise created by a breakfast sandwich makes the data useless. Precision requires a blank slate.
Which Tests Require Fasting? (The Definitive Breakdown)
Not all vials of blood are created equal. The necessity of the fast depends entirely on the analyte stability. It depends on the specific marker your doctor ordered. Here is the breakdown of common panels.
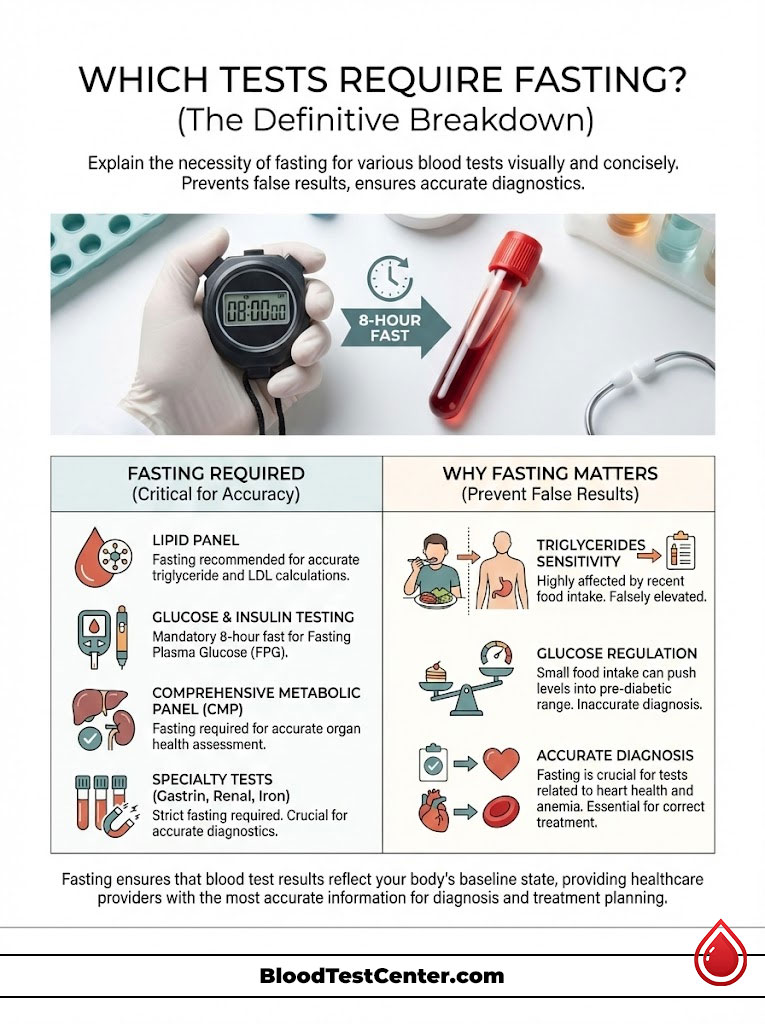
The Lipid Panel (Cholesterol & Triglycerides)
There has been significant debate recently regarding lipid panel fasting. The American College of Cardiology (ACC) has suggested that for general screening, non-fasting samples are acceptable. However, as a pathologist, I advise caution here.
Total Cholesterol and HDL are relatively stable after a meal. However, triglycerides are not. They are extremely sensitive to food. If you eat, your triglycerides spike significantly.
The LDL (Bad Cholesterol) is often calculated using a formula. This is called the Friedewald equation. It relies on the triglyceride count. A false high triglyceride count leads to a false low LDL calculation. For the most accurate cardiac risk assessment, the 12-hour fast remains the gold standard.
Glucose and Insulin Testing
This is non-negotiable. For a Fasting Plasma Glucose (FPG) test, you must abstain from calories for at least 8 hours. The range for pre-diabetes is tight. It sits between 100 and 125 mg/dL.
A single piece of fruit can push a healthy person into that range temporarily. If you are taking an Oral Glucose Tolerance Test (OGTT), strict protocols apply. You must arrive fasting to establish a baseline.
Comprehensive Metabolic Panel (CMP)
The Comprehensive Metabolic Panel is a broad sweep of your organ health. It looks at your liver, kidneys, electrolytes, and fluid balance. Glucose is a core component of this panel.
Therefore, the entire test generally defaults to a fasting requirement. Additionally, the liver enzymes (AST and ALT) can be affected by lipemia. Bilirubin measurements are also sensitive to light transmission issues caused by fat. Fasting is the safest route to ensure every number on this 14-point inspection is accurate.
Specialty Tests
There are several specialized tests that demand a strict fast. Gastrin is a hormone involved in stomach acid production. Eating causes it to skyrocket. Fasting is mandatory for diagnosis.
Renal Function Panels often require fasting. This helps get an accurate baseline of phosphorus and urea nitrogen. Iron studies are another major category.
Iron levels fluctuate rapidly. They are highest in the morning and drop after eating. Fasting for blood work involving iron is essential. It is the only way to diagnose anemia properly.
Tests That Do Not Require Fasting
We often see patients starving themselves unnecessarily. Some tests are completely unaffected by lunch. Understanding which is which can save you a lot of hunger pangs.
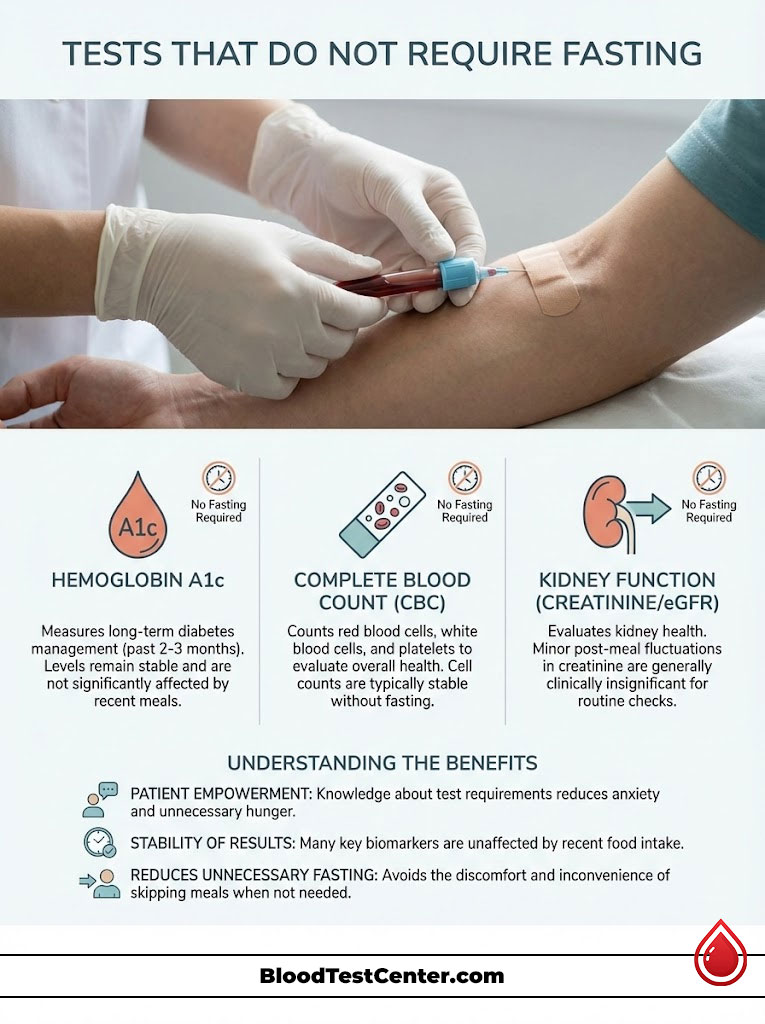
Hemoglobin A1c
This is the primary marker for long-term diabetes management. Hemoglobin A1c measures the amount of sugar attached to your red blood cells. It looks at the average over their 3-month lifespan.
Because it represents a 90-day average, a donut eaten one hour ago has zero impact on the result. You do not need to fast for an A1c. It is a stable historical record.
Complete Blood Count (CBC)
This test counts your cells. It looks at Red blood cells, White blood cells, and Platelets. These cellular components are stable.
A heavy fatty meal might cause slight interference due to turbidity. However, a standard CBC is generally considered a non-fasting test. Your cell counts do not change drastically with digestion.
Kidney Function (Creatinine/eGFR)
Creatinine levels are fairly stable when ordered in isolation. This is often done for contrast dye clearance checks. However, a meal extremely high in cooked meat can temporarily bump creatinine levels slightly.
This is due to the breakdown of muscle protein in the meat. For the average person, though, fasting is not required. The fluctuation is usually clinically insignificant.
Detailed Comparison: Fasting vs. Non-Fasting Protocols
To help clarify the confusion, here is a comparison of the standard of care for common tests. This table outlines why the rules exist.
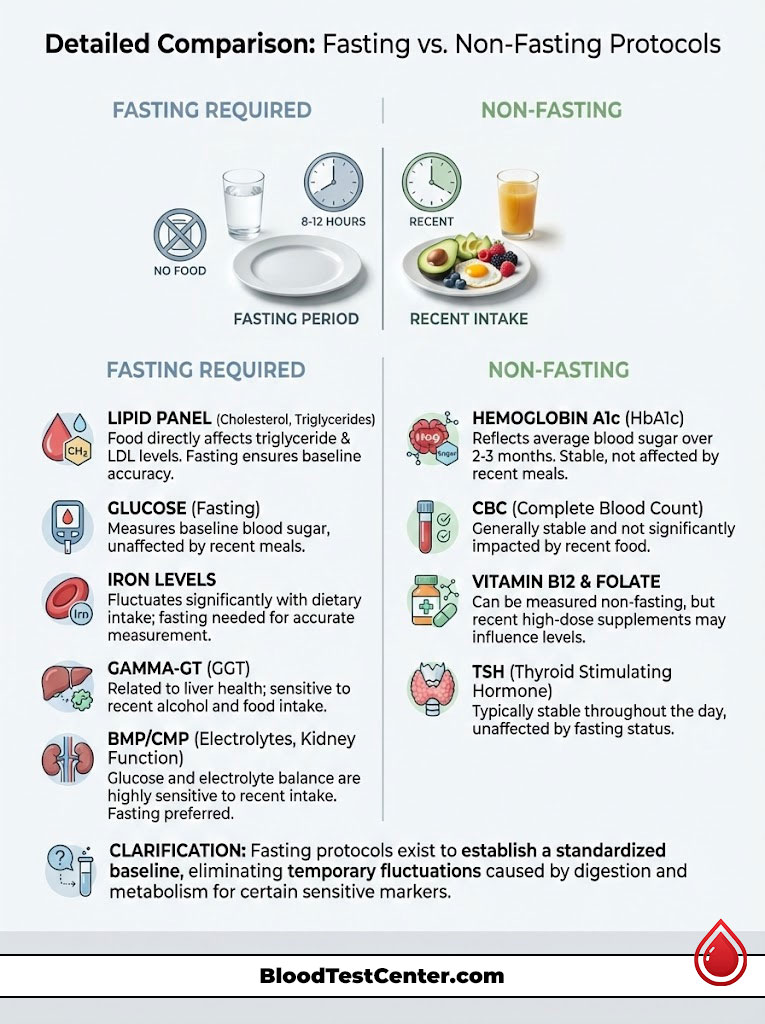
| Test Name | Standard Requirement | Pathologist’s Note on Physiology |
|---|---|---|
| Lipid Panel | 9–12 Hours Fasting | Triglycerides spike significantly post-meal. This alters LDL calculations. |
| CMP / BMP | 8–10 Hours Fasting | Glucose and electrolyte balance are sensitive to recent intake. |
| Hemoglobin A1c | Non-Fasting | Measures long-term glycation. It is unaffected by recent meals. |
| Iron Studies | 12 Hours Fasting | Iron levels fluctuate rapidly throughout the day and after eating. |
| Vitamin B12 / Folate | 6–8 Hours Fasting | Recent intake can temporarily elevate serum levels. This masks deficiency. |
| Gamma-GT (Liver) | 8 Hours Fasting | Highly sensitive to alcohol and food intake. |
The “Grey Area” Substances: Water, Coffee, and Gum
This is where patients get tripped up most often. The definition of “nothing by mouth” seems flexible to the layperson. However, chemistry is rigid.
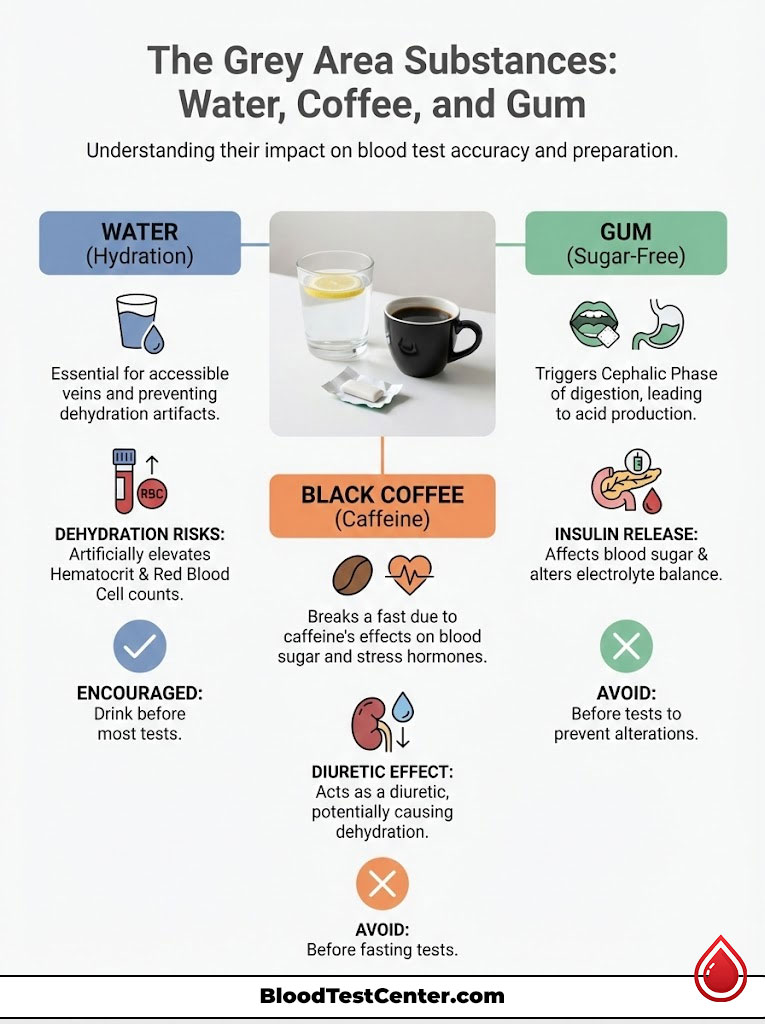
Hydration is Critical
One of the most common questions is whether you can drink water. The answer is a resounding yes. In fact, we encourage it.
Hydration serves two purposes. First, it makes your veins turgid and accessible. This makes the phlebotomy experience faster and less painful. Second, it prevents dehydration artifacts.
If you are dehydrated, your blood volume decreases. However, the cellular mass stays the same. This is called hemoconcentration. It can artificially elevate your Hematocrit and Red Blood Cell count. It can also raise BUN (Blood Urea Nitrogen). Doctors may think you have kidney issues when you are just thirsty.
The Coffee Debate
Does black coffee break a fast for blood work? Yes, it does. Many patients assume that because black coffee has no calories, it is neutral. Physiologically, this is incorrect.
Caffeine is a potent stimulant. It triggers your adrenal glands to release epinephrine and cortisol. These stress hormones signal the liver to release stored glycogen into the bloodstream as glucose.
So, even without sugar in the cup, coffee before blood test appointments can spike your blood sugar. It skews your cortisol results. It also acts as a diuretic. This potentially causes the dehydration issues mentioned above.
Chewing Gum and Mints
Even sugar-free gum is a problem. The act of chewing triggers the “Cephalic Phase” of digestion. Your brain tells your stomach that food is coming.
Your stomach produces acid. Your pancreas may release a small amount of insulin in anticipation. This can lower your blood sugar slightly. It can alter your electrolyte balance. Avoid the gum.
Medications and Supplements: The Hidden Interferents
While food is the obvious culprit, what you take from your medicine cabinet can be just as disruptive. We need to account for pharmaceutical interference.
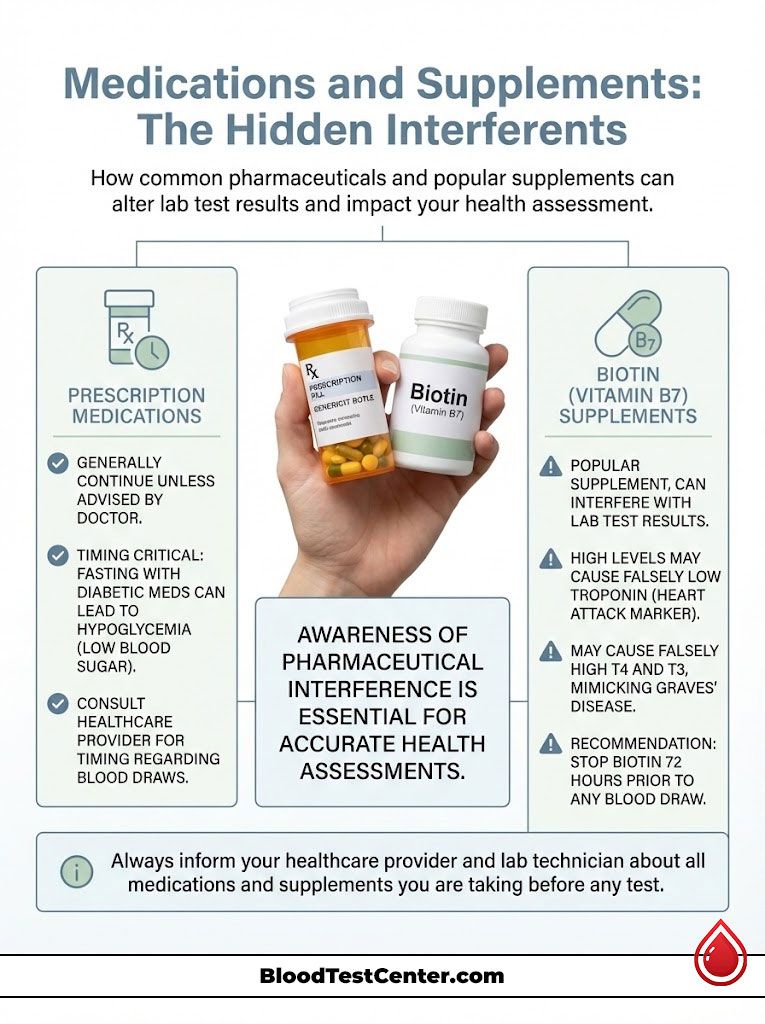
Prescription Medications
The general rule is to continue taking your prescription medications. Do this unless your doctor specifically tells you to stop. However, timing is everything.
If you are on diabetic medication, taking it while fasting could cause your blood sugar to crash. This results in hypoglycemia. Always coordinate with your provider regarding the timing of your draw relative to your morning dose.
The Biotin (Vitamin B7) Problem
This is a critical safety warning. Biotin is popular for hair and nail growth. However, biotin interference in lab tests is a major issue in modern pathology.
Many lab tests use biotin-streptavidin technology to bind and measure chemicals. If you have high levels of biotin in your blood, it interferes with the assay. This causes falsely low results for Troponin, a heart attack marker.
It can also cause falsely high results for T4 and T3. This can mimic Graves’ disease. We recommend stopping Biotin supplements 72 hours before any blood draw.
Value-Add Comparison: Impact of “Cheating” on Results
So, what happens if I eat before a blood test? It depends on what you consumed. Here is the physiological impact of breaking the fast.
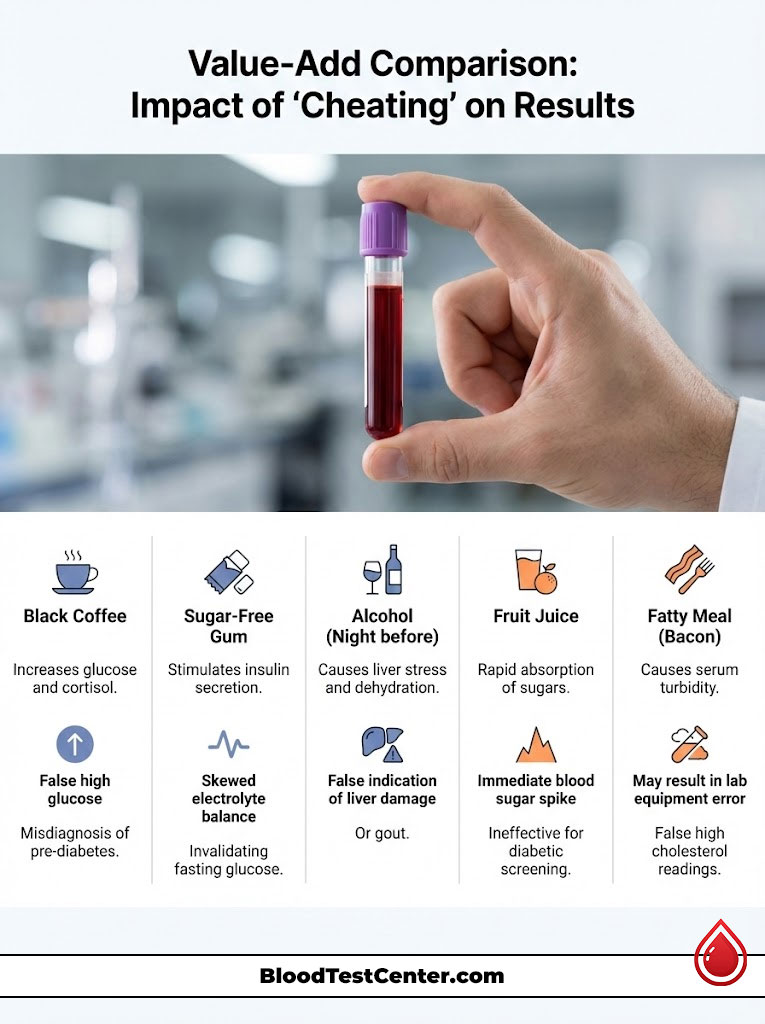
| Consumed Item | Affected Analyte | Physiological Mechanism | Potential Consequence |
|---|---|---|---|
| Black Coffee | Glucose, Cortisol | Caffeine stimulates adrenal glands and liver glycogen release. | False high glucose; Misdiagnosis of pre-diabetes. |
| Sugar-Free Gum | Insulin, Chloride | Chewing stimulates digestive enzymes and insulin secretion. | Skewed electrolyte balance; Invalidated fasting glucose. |
| Alcohol (Night before) | GGT, Triglycerides | Liver stress response and dehydration. | False indication of liver damage or gout. |
| Fruit Juice | Glucose, Potassium | Rapid absorption of simple sugars. | Immediate spike in blood sugar; useless for diabetic screening. |
| Fatty Meal (Bacon) | Triglycerides, Bilirubin | Chylomicron shower causes serum turbidity (lipemia). | Lab equipment error; sample rejection; false high cholesterol. |
Guidelines for Special Populations
Fasting is not one-size-fits-all. Different bodies handle metabolic stress differently. We must adapt protocols for specific groups.
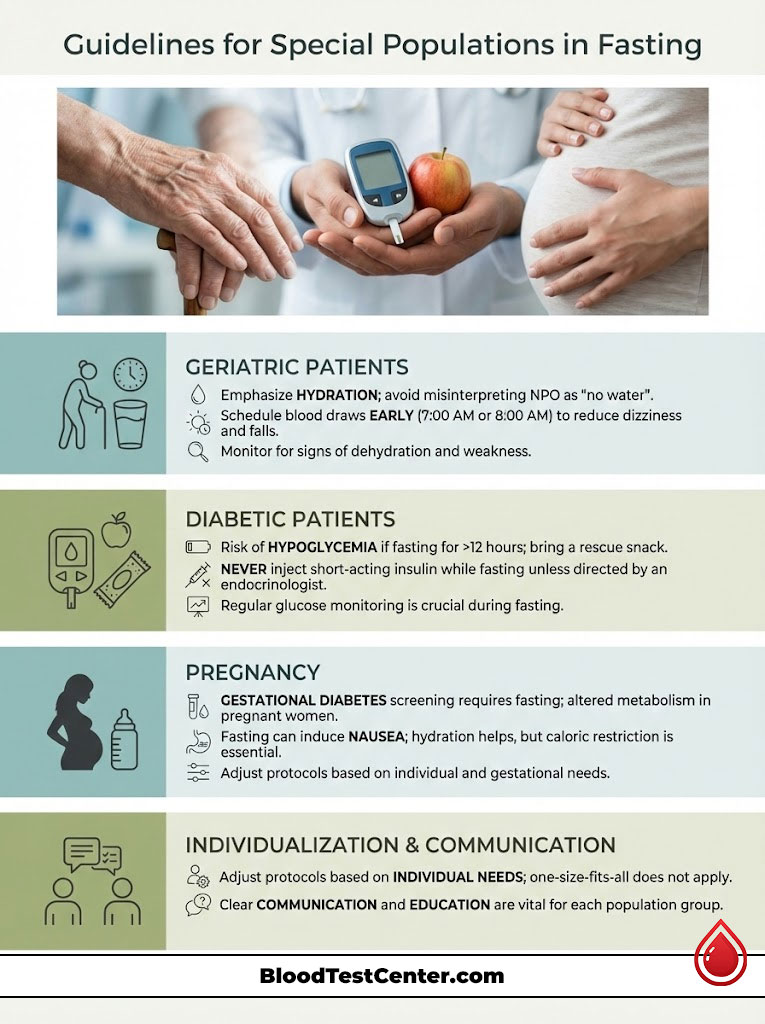
Geriatric Patients
Elderly patients are more prone to dehydration. For them, the NPO instruction is often misinterpreted as “no water.” It is vital to emphasize hydration.
Furthermore, long fasts can cause dizziness and falls in this population. We often try to schedule geriatric draws as early as possible. Typically, we aim for 7:00 AM or 8:00 AM.
Diabetic Patients
This is the most delicate balance. A diabetic patient on insulin who fasts for 12 hours runs a real risk of hypoglycemia. This can be dangerous.
If you are diabetic, bring a rescue snack like juice or glucose tabs to the appointment. Take it immediately after the blood is drawn. Never inject short-acting insulin while fasting unless specifically instructed by your endocrinologist.
Pregnancy
Gestational diabetes screening is a standard part of prenatal care. The Glucose Tolerance Test requires a fasting baseline. Pregnant women have altered metabolism.
Fasting can induce nausea more quickly in pregnant patients. Hydration helps mitigate the nausea. However, the caloric restriction remains necessary for the safety of the pregnancy and accuracy of the test.
The Impact of Exercise and Stress
It is not just about food. Your activity level before the test matters significantly. Physical stress changes blood chemistry.
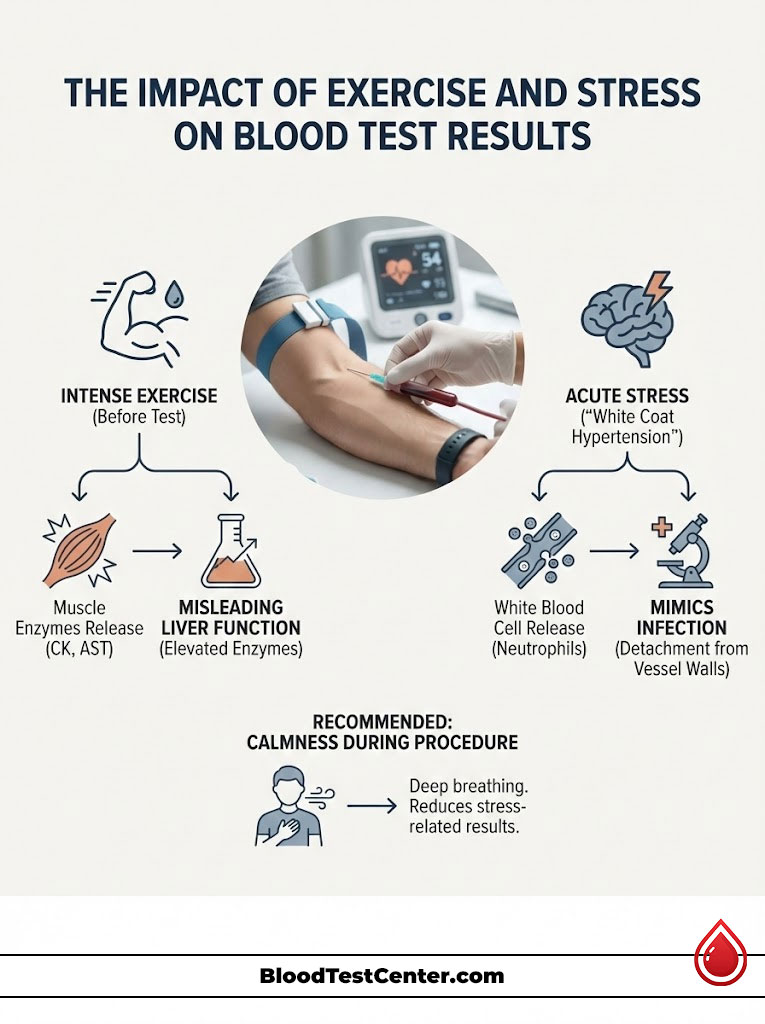
Exercise Interference
Patients often ask if they can exercise the morning of a blood test. The answer is generally no. Intense activity releases muscle enzymes.
Creatine Kinase (CK) and AST are released from muscle tissue during workouts. If you run a 5K before your appointment, your liver enzymes might look elevated. This could lead a doctor to suspect liver damage when it is actually just muscle recovery.
The Stress Response
Anxiety about the needle itself can alter results. This is known as “White Coat Hypertension,” but it applies to blood chemistry too. Acute stress raises White Blood Cell counts.
It triggers a demargination of neutrophils. This means white blood cells detach from blood vessel walls and enter the stream. It can mimic an infection. Try to stay calm and breathe deeply during the procedure.
Advanced Lipidology: Beyond the Basics
We touched on lipids earlier, but the nuance here is deep. The debate about fasting for lipids centers on LDL. This is the “bad” cholesterol.
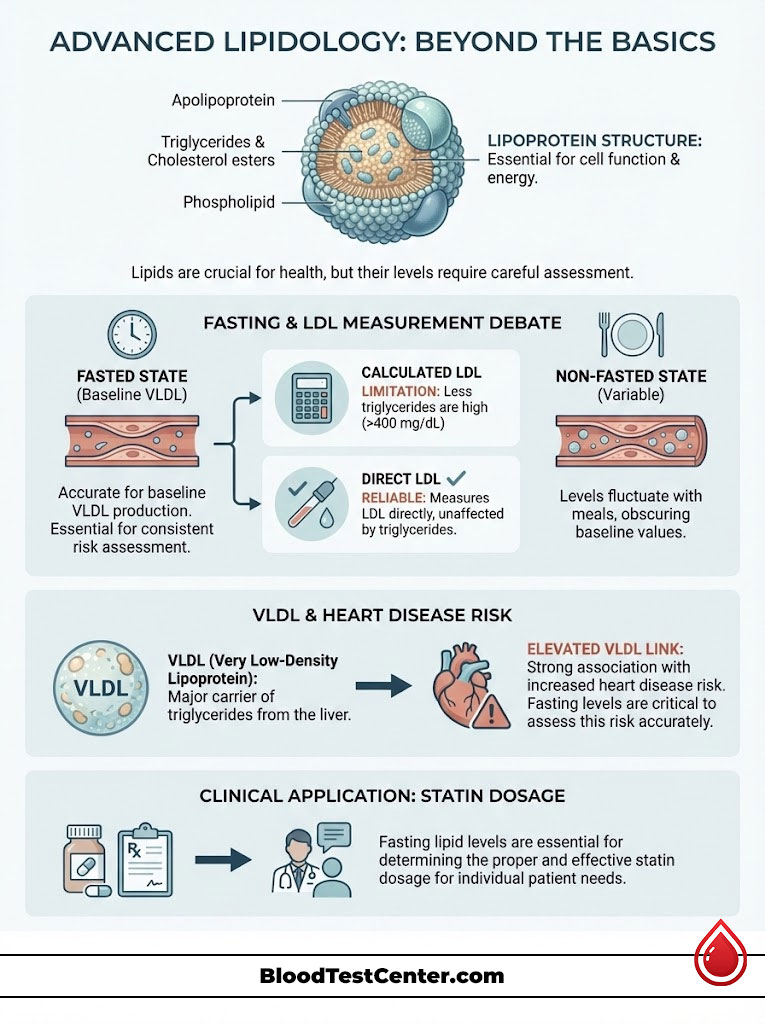
Direct LDL vs. Calculated LDL
Most standard lab panels use a calculation for LDL. We measure Total Cholesterol, HDL, and Triglycerides. We then use math to estimate the LDL.
This formula fails if triglycerides are high. If you eat, triglycerides rise. This makes the math wrong. Some advanced labs measure Direct LDL. This method measures the particle directly.
If your doctor orders a Direct LDL, fasting is less critical. However, you likely will not know which test is ordered until you arrive. Therefore, fasting remains the safest bet to ensure the calculation is valid.
VLDL and Chylomicrons
Very Low-Density Lipoprotein (VLDL) is another carrier of fat. It is tightly linked to your recent meal. High levels of VLDL are a risk factor for heart disease.
Fasting allows us to see your baseline VLDL production. This is the amount your liver produces naturally. It separates it from the fat you just ate. This distinction helps in prescribing the right statin dosage.
The Role of Circadian Rhythms
Your body is a clock. Every cell has a rhythm. Blood tests are snapshots in time. We need to take that snapshot when the lighting is right.
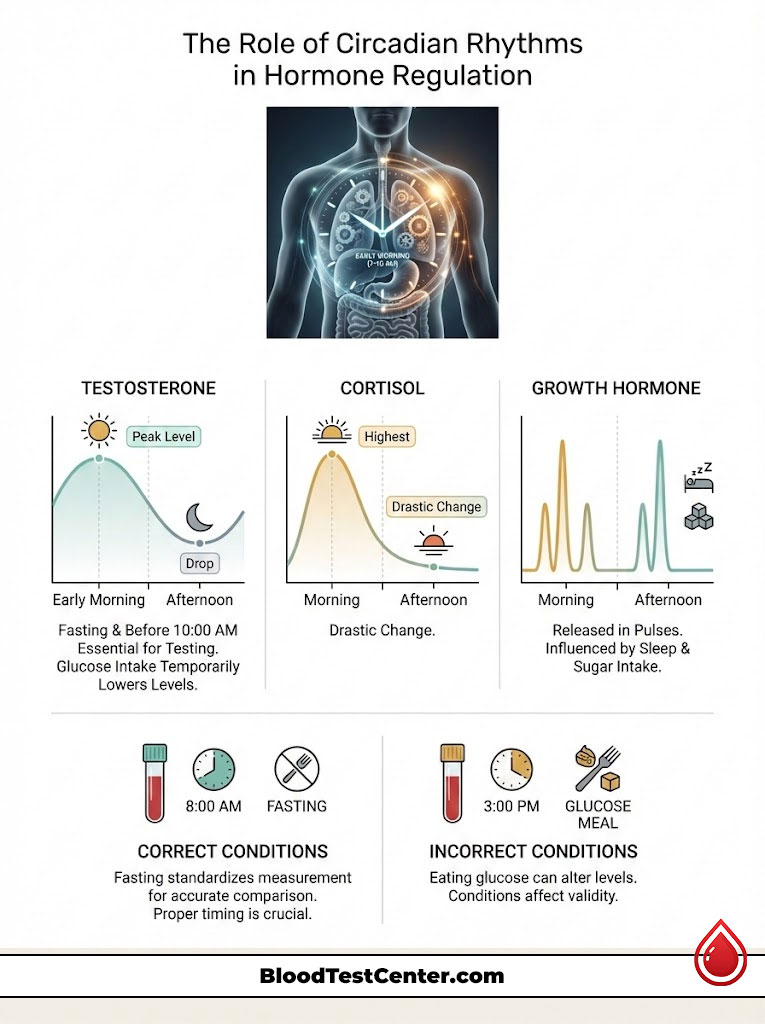
Testosterone Testing
Testosterone levels follow a strict diurnal variation. They are highest in the early morning. They drop significantly by the afternoon.
Eating glucose can also suppress testosterone levels temporarily. For an accurate diagnosis of hypogonadism (Low T), the blood must be drawn fasting. It must also be drawn before 10:00 AM. A draw at 3:00 PM after lunch will almost always show low levels.
Growth Hormone and Cortisol
Growth hormone is released in pulses. It is affected by sleep and sugar. Cortisol is the waking hormone. It helps you get out of bed.
If we measure cortisol in the afternoon, the reference ranges change completely. Fasting helps standardize these variables. It ensures we are comparing your levels to a valid standard.
What to Do If You Accidentally Break the Fast
It happens. You wake up groggy. You walk to the kitchen. You eat a cookie before remembering your appointment. If you have accidentally eaten before a blood test, what should you do?
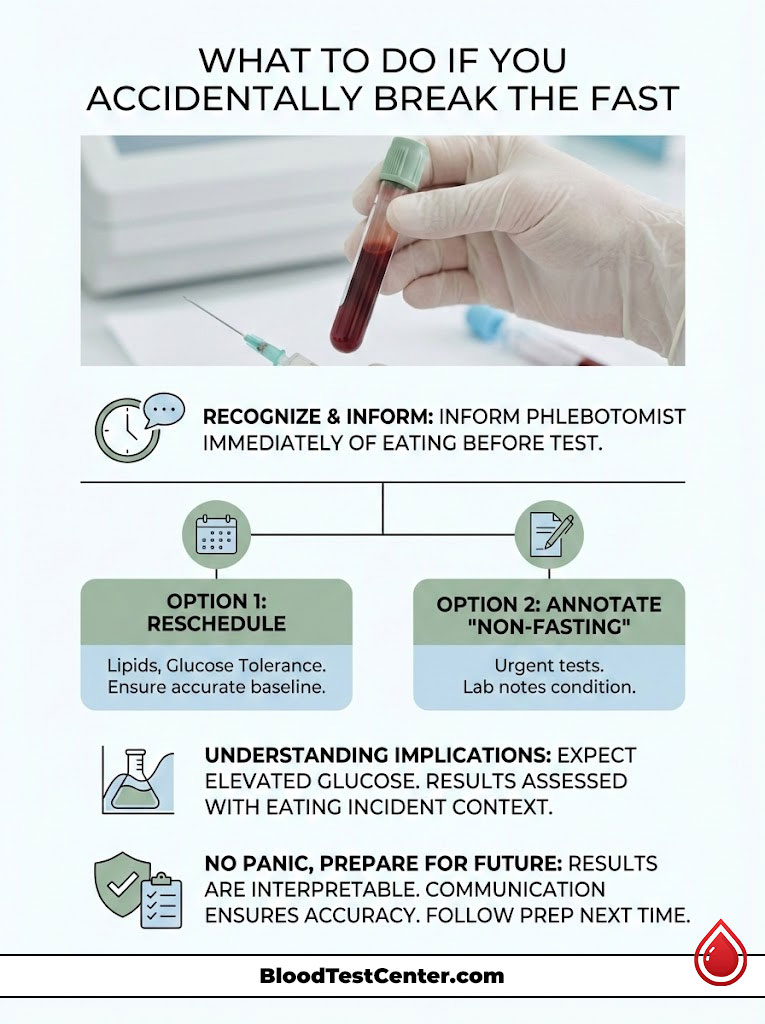
Honesty is the only policy. Do not try to hide it. As I mentioned, the lipemia in your serum will likely give you away. Your glucose will be surprisingly high.
Tell the phlebotomist immediately. They have two options. First, they can reschedule. If the test is strictly for lipids or glucose tolerance, rescheduling is the medically responsible choice.
Second, they can annotate. If the blood work is urgent, the phlebotomist can write “Non-Fasting” on the requisition. When I receive that sample in the lab, I will interpret the results with that context. I won’t flag a glucose of 130 mg/dL as alarming if I know you just had a bagel.
The Future of Fasting: Will It Become Obsolete?
Science is evolving. We are developing better assays. We are creating tests that are less sensitive to interference. The movement toward non-fasting lipid panels is one example.
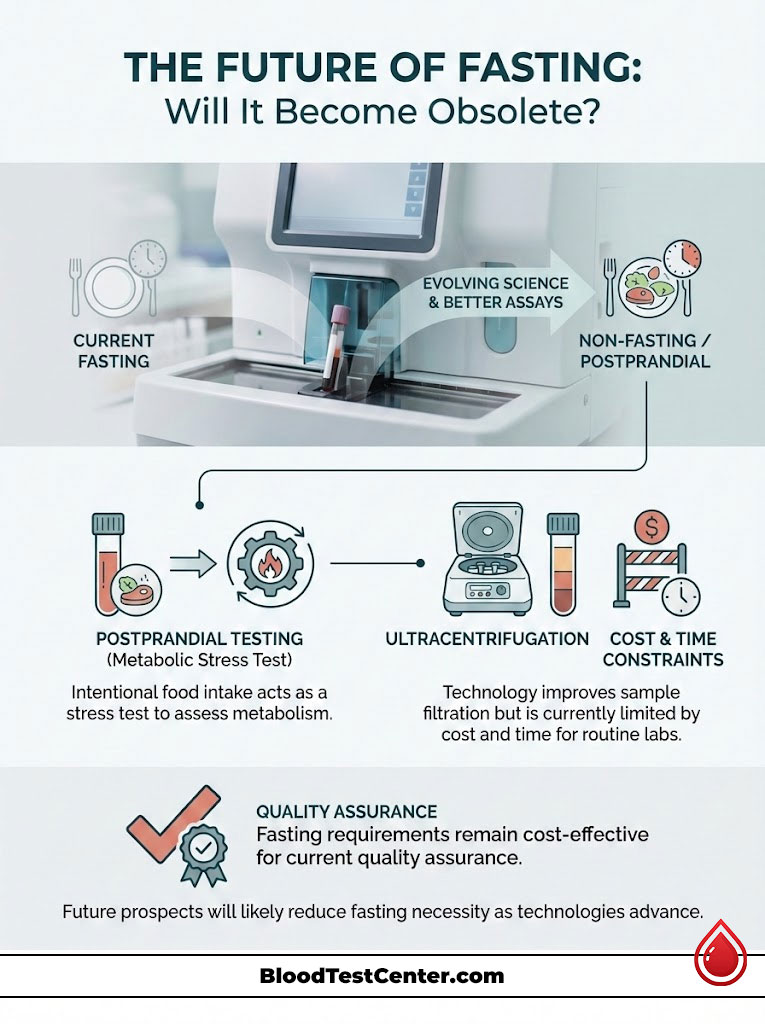
Postprandial Testing
Some doctors are now interested in how your body handles food. They want to see the spike. This is called postprandial testing. It is intentional.
In these cases, you are instructed to eat. This is a stress test for your metabolism. However, this is a specific diagnostic tool. It is not the standard for a routine annual physical.
Technological Advances
Newer analyzers have better filtration. They can sometimes clear lipemia from a sample before testing. This is called ultracentrifugation. However, it is expensive and time-consuming.
Most routine labs do not perform this on every sample. Until this technology is universal, the fasting requirement will likely remain. It is the most cost-effective way to ensure quality.
Summary & Key Takeaways
So, is it necessary to fast before a routine blood test? Yes, if you want results you can trust. While technology is improving and some organizations are relaxing guidelines for general screening, the biochemistry of the human body has not changed. Food introduces variables like sugar, fat, and hormonal shifts that cloud the diagnostic picture.
- The Safe List: Water is your friend. Drink plenty of it to keep veins accessible.
- The Ban List: Avoid coffee (even black), tea, alcohol, gum, mints, and all food.
- The Timing: 8–12 hours is the standard window to reach a basal state.
- The Why: We fast to clear postprandial glucose spikes. We also fast to eliminate lipemic serum that interferes with lab instruments.
When in doubt, fast. It is better to be slightly hungry for a morning than to undergo expensive, anxiety-inducing repeat testing. Do not let a breakfast sandwich skew your data. Your health is worth the wait.
Frequently Asked Questions
Why is a basal state necessary for accurate diagnostic testing?
Reaching a basal state through an 8–12 hour fast ensures that metabolic markers like glucose and triglycerides have stabilized after the chemical noise of digestion. This allows pathologists to compare your results against standardized reference ranges without interference from recent dietary intake, preventing clinical misdiagnosis.
Does drinking black coffee before a fasting blood test affect the results?
Yes, caffeine is a potent stimulant that triggers the adrenal glands to release cortisol and epinephrine, which signals the liver to release stored glycogen as glucose. Even without sugar or cream, coffee can cause a 10–15% false elevation in blood sugar and skew hormonal markers, often requiring a sample rejection.
Is water consumption permitted during the fasting period for blood work?
Abundant water consumption is highly encouraged because hydration makes your veins more accessible for the phlebotomist and prevents hemoconcentration. Dehydration can artificially inflate red blood cell counts and kidney markers like Blood Urea Nitrogen (BUN), leading to an inaccurate picture of renal health.
How does eating a fatty meal impact the accuracy of a lipid panel?
Dietary fats create chylomicrons that cause lipemia, or cloudy serum, which interferes with the light-based spectrophotometry used by lab analyzers. Furthermore, postprandial triglyceride spikes can lead to an inaccurately low calculated LDL value when using the Friedewald equation, compromising your cardiac risk assessment.
Why must I stop taking Biotin supplements 72 hours before laboratory testing?
High-dose Biotin (Vitamin B7) interferes with the biotin-streptavidin technology used in many modern immunoassays to measure chemicals. This interference can cause dangerously false results, such as masking a heart attack by lowering Troponin readings or mimicking Graves\’ disease by inflating thyroid hormone levels.
Does a Hemoglobin A1c test require fasting?
No, the Hemoglobin A1c measures the average glycation of red blood cells over their 90-day lifespan, making it a stable historical record of blood sugar. Because it reflects long-term glucose management rather than immediate metabolic shifts, a recent meal has zero impact on the final percentage.
Can I exercise on the morning of my routine blood draw?
It is best to avoid intense physical activity as exercise can cause transient elevations in muscle enzymes like Creatine Kinase (CK) and liver enzymes like AST. These spikes can be misinterpreted by your physician as organ damage or pathology rather than normal physiological muscle recovery.
What happens if I chew sugar-free gum before a fasting lab test?
Chewing gum triggers the cephalic phase of digestion, causing the brain to signal the release of stomach acid and insulin in anticipation of food. These physiological responses can shift your electrolyte balance and lower your fasting glucose baseline, potentially invalidating the accuracy of metabolic screenings.
Why is timing critical for testosterone and growth hormone blood tests?
These hormones follow a strict diurnal rhythm and are naturally at their peak in the early morning hours. Testing later in the day or after a meal—which can acutely suppress testosterone—may result in a false diagnosis of hypogonadism or hormonal deficiency when compared to standard reference ranges.
What should I do if I accidentally ate before my scheduled fasting blood test?
You must inform your phlebotomist immediately so they can either reschedule the appointment or annotate the sample as \”non-fasting\” for the pathologist. Transparency is vital to prevent clinical misinterpretation of elevated glucose or triglycerides that could lead to unnecessary and potentially harmful prescriptions.
Should I take my morning medications before a fasting blood draw?
Generally, you should continue your prescription regimen unless specifically instructed otherwise, but timing is crucial for diabetic patients. Taking insulin or oral hypoglycemics while fasting can lead to severe hypoglycemia; always coordinate the timing of your draw with your healthcare provider to ensure safety.
Why do iron studies and Vitamin B12 tests require a fast?
Serum iron and B12 levels are highly sensitive to recent dietary intake and can fluctuate rapidly throughout the day based on caloric absorption. Fasting ensures we capture your true baseline levels, preventing a temporary post-meal spike from masking a legitimate nutritional deficiency or underlying anemia.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The information provided is intended to help patients understand general laboratory protocols. Always consult with your primary healthcare provider or the specific laboratory performing your tests for exact instructions tailored to your medical history and specific diagnostic needs.
References
- American Association for Clinical Chemistry (AACC) – aacc.org – Providing expert guidelines on Biotin interference and standardized fasting protocols for metabolic testing.
- American College of Cardiology (ACC) – acc.org – Source for the latest clinical perspectives on fasting vs. non-fasting lipid panels for cardiovascular risk.
- Clinical and Laboratory Standards Institute (CLSI) – clsi.org – The global leader in developing clinical laboratory standards, including venipuncture and pre-analytical variables.
- Mayo Clinic Laboratories – mayocliniclabs.com – Comprehensive test catalog detailing the physiological impact of food on glucose and hormone analytes.
- Journal of Clinical Pathology – jcp.bmj.com – Peer-reviewed research regarding the effects of lipemia and turbidity on spectrophotometric laboratory analyzers.

