In the context of a routine Comprehensive Metabolic Panel (CMP), an elevated ALT (Alanine Aminotransferase) level typically indicates that liver cells are experiencing stress, inflammation, or injury. When liver cells (hepatocytes) are damaged, they release this specific enzyme into the bloodstream. While often triggered by benign factors like medication use or mild fatty liver, it serves as a crucial signal for physicians to investigate metabolic health further.
Table of Contents
You open your secure patient portal to check your annual physical results. You scroll past the normal numbers for sodium, potassium, and glucose until you stop at a red flag. An exclamation point sits next to a specific acronym.
Your ALT (Alanine Aminotransferase) is elevated.
For millions of Americans, this moment triggers immediate anxiety. You likely feel perfectly healthy. You have no abdominal pain. You fasted for 12 hours exactly as the nurse instructed. Yet the numbers suggest something is wrong with your liver.

Before you spiral into a worst-case scenario, it is vital to understand the clinical context of this finding. An elevated ALT in a routine panel is one of the most common abnormalities seen in primary care medicine today. In the vast majority of cases discovered during an asymptomatic preventive screening, it does not point to immediate organ failure. Instead, it serves as a metabolic “check engine” light. It is a conversation starter between your body and your doctor about inflammation, lifestyle, and how your liver is processing the modern environment.
This comprehensive guide will break down exactly what that number represents, why it appears in your Comprehensive Metabolic Panel, and the specific, evidence-based steps healthcare providers take to interpret and address it.
Understanding the Biology of Alanine Aminotransferase (ALT) and Liver Function
To truly grasp why your levels are high, you first need to understand the biological mechanics of this enzyme. Alanine Aminotransferase (ALT) is not a toxin itself. It is a worker protein. It acts as a vital catalyst for chemical reactions within your body, primarily facilitating the conversion of proteins into energy for your liver cells.
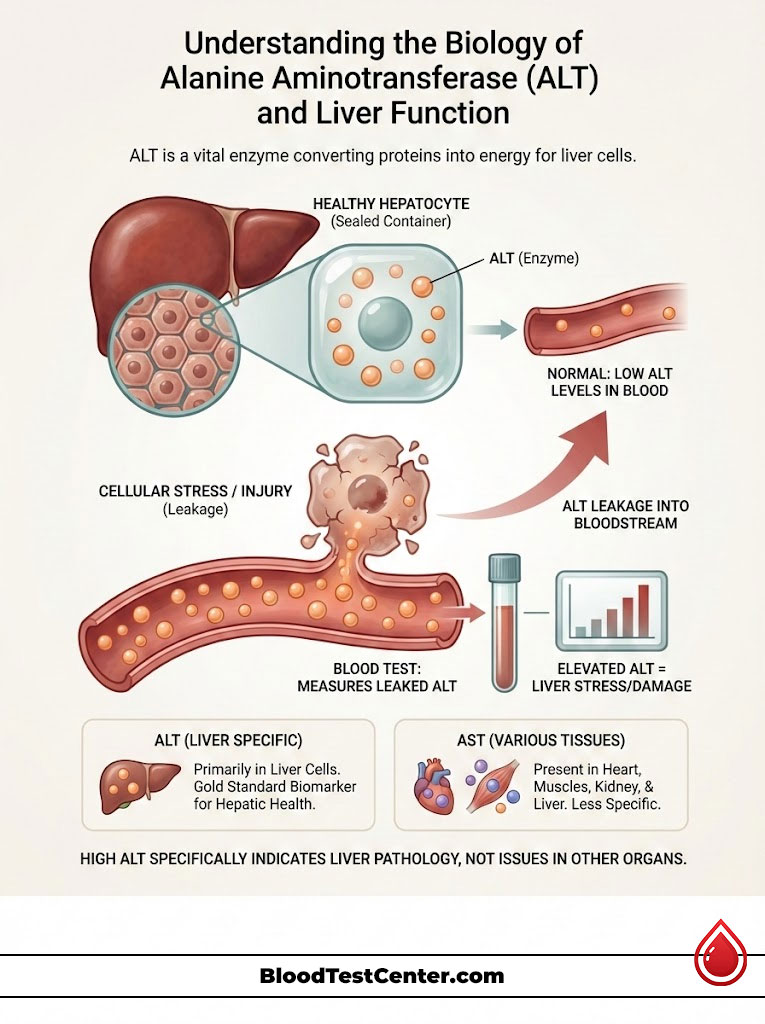
The Cellular Leakage Mechanism in Hepatocytes
Think of your liver cells, medically known as hepatocytes, as sealed containers holding this enzyme. Under normal homeostatic conditions, the ALT stays inside these cells where it performs its metabolic duties. The concentration of the enzyme in your blood should remain very low.
However, hepatocytes are sensitive. When the cell wall of a liver cell is stressed, inflamed, or injured, the membrane becomes permeable. The “container” develops microscopic cracks. Consequently, the enzyme leaks out of the cell and spills into your blood plasma.
When a lab technician runs your CMP blood test, they are measuring the amount of this leaked enzyme floating in your serum. Therefore, the level of ALT in your blood is directly proportional to the amount of cellular stress or death (necrosis) occurring in the liver at that moment. The higher the number, the more cells are “leaking.”
Why ALT is Considered a Liver-Specific Biomarker
You will often see ALT measured alongside another enzyme called AST (Aspartate Aminotransferase). While they are often grouped together as “liver enzymes,” they tell different stories.
AST is found in various tissues throughout the body, including the heart, skeletal muscles, kidneys, and brain. If you run a marathon, your AST might rise because of muscle stress. ALT, conversely, is found almost exclusively in the liver. This high specificity makes Alanine Aminotransferase the gold standard for hepatic health. If it is high, the problem is almost certainly originating in the liver, rather than the heart or muscles. This specificity is why it is the primary focus when screening for liver pathology in a routine metabolic panel.
The Role of the Routine Comprehensive Metabolic Panel (CMP) in Preventive Health
Your doctor likely did not order a “liver test” specifically. They ordered a Comprehensive Metabolic Panel. It is crucial to understand the difference to contextualize your results.
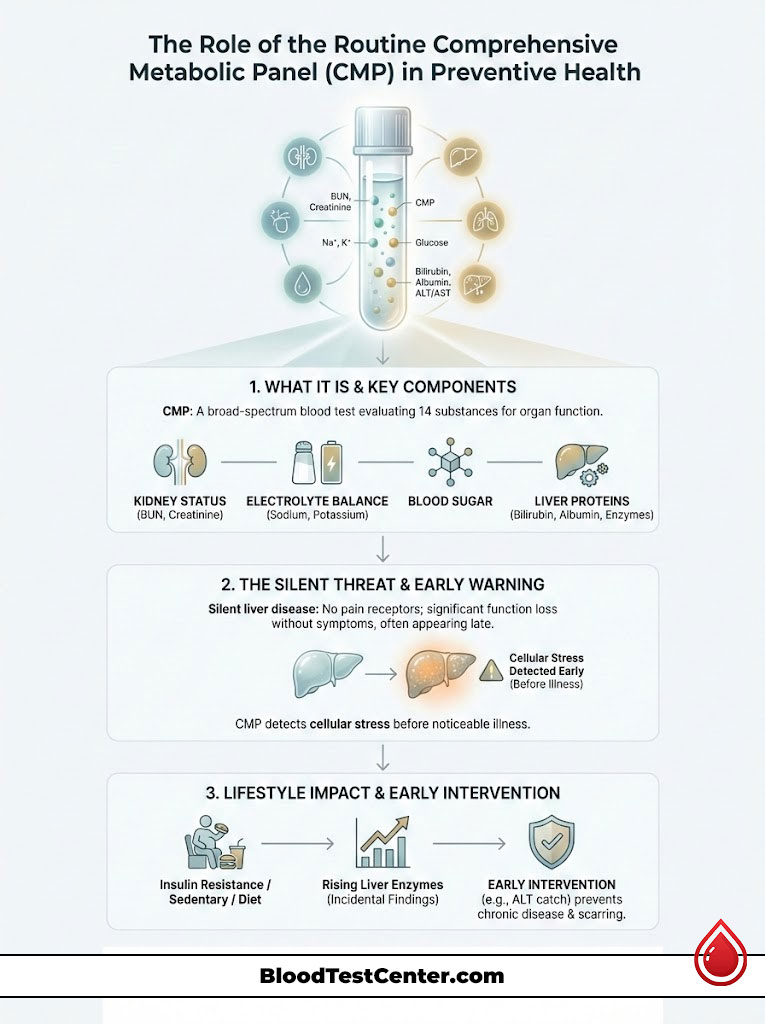
A CMP blood test is a broad-spectrum screening tool that measures 14 different substances in your fluid to evaluate overall organ function. It provides a snapshot of your kidney status (BUN, Creatinine), your electrolyte balance (Sodium, Potassium), your blood sugar, and your liver proteins (Bilirubin, Albumin, Enzymes).
Detecting Silent Liver Disease in Asymptomatic Patients
The liver is often referred to as a “silent” organ. Unlike the stomach or the heart, the liver has no pain receptors inside its tissue. The capsule surrounding the liver has nerves, but the organ itself does not. This means you can lose a significant percentage of liver function without ever feeling a specific ache in your right upper quadrant.
Classic symptoms of liver disease, such as jaundice (yellowing of the eyes), ascites (fluid retention), or easy bruising, typically do not appear until the disease has reached an advanced, often irreversible stage. Therefore, the routine metabolic panel acts as the only reliable early warning system. It detects cellular stress on a microscopic level long before you feel sick.
Incidental Findings of High Liver Enzymes in the USA
In the United States healthcare system, we are witnessing a massive rise in “incidental” findings of elevated liver enzymes. An incidental finding is a medical anomaly discovered by accident when looking for something else, or during a standard checkup.
This shift is largely driven by metabolic factors common in the US population, specifically the rise in insulin resistance, sedentary lifestyles, and dietary trends. By catching an elevated ALT in a routine panel early, physicians can intervene years, or even decades, before permanent scarring (cirrhosis) occurs. It shifts the focus from treating sickness to preventing chronic disease.
Analyzing Normal Ranges vs. Elevated ALT Levels in a CMP
Interpreting your result requires a nuanced understanding of what “normal” actually looks like in a diverse population. In the USA, laboratory reference ranges are determined by analyzing samples from thousands of “healthy” individuals and finding the statistical average. However, these ranges can vary slightly between major commercial labs like Labcorp, Quest Diagnostics, and hospital-based pathology departments.
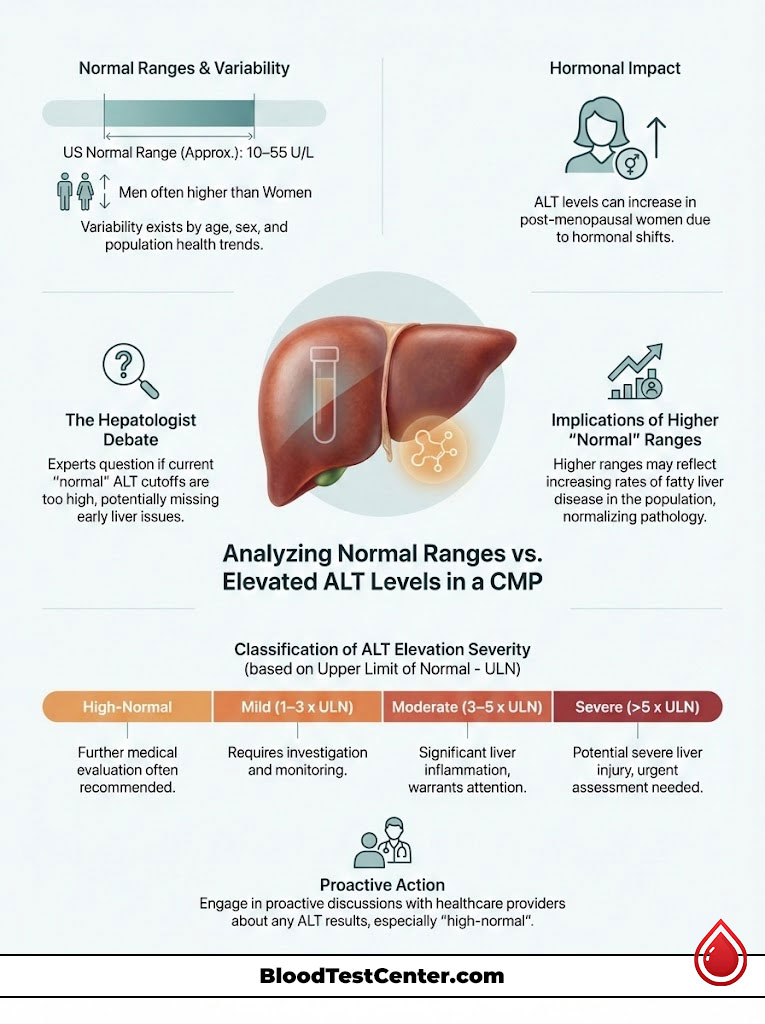
Standard Reference Ranges for Men and Women in Major US Labs
For Alanine Aminotransferase, there is a distinct gender gap due to differences in muscle mass and hormonal profiles.
- Males: 29 to 33 units per liter (U/L) is often considered the upper limit of optimal health, though some standard lab reports may accept levels up to 55 U/L as “normal.”
- Females: 19 to 25 U/L is optimal, with some labs accepting up to 45 U/L.
It is important to note that men generally have higher baseline levels. However, post-menopausal women may see a slight natural increase in their baseline enzymes due to hormonal shifts, which doctors take into account.
The Medical Debate: Defining True “Normal” vs. “Average” ALT
There is a growing consensus among hepatologists (liver specialists) that the standard “normal” cutoff on your printed lab report might be too high.
The American College of Gastroenterology has suggested that true healthy limits should be lower than what many labs currently list. This is because the “average” American population used to create the baseline has become heavier and more metabolically unwell over the last two decades. If the reference group includes people with undiagnosed fatty liver, the “normal” range skews higher.
Consequently, if your lab report says “Normal” but your number is 45 U/L, you might still have low-grade liver inflammation. This is why a “high-normal” result often triggers a conversation with a proactive physician.
Classification of Elevation Severity
Doctors categorize elevated ALT in a routine panel based on the magnitude of the increase relative to the upper limit of normal (ULN).
Comparison Table: Interpreting Severity of Elevation
The following table breaks down how clinical guidelines categorize the urgency of elevated ALT in a routine panel.
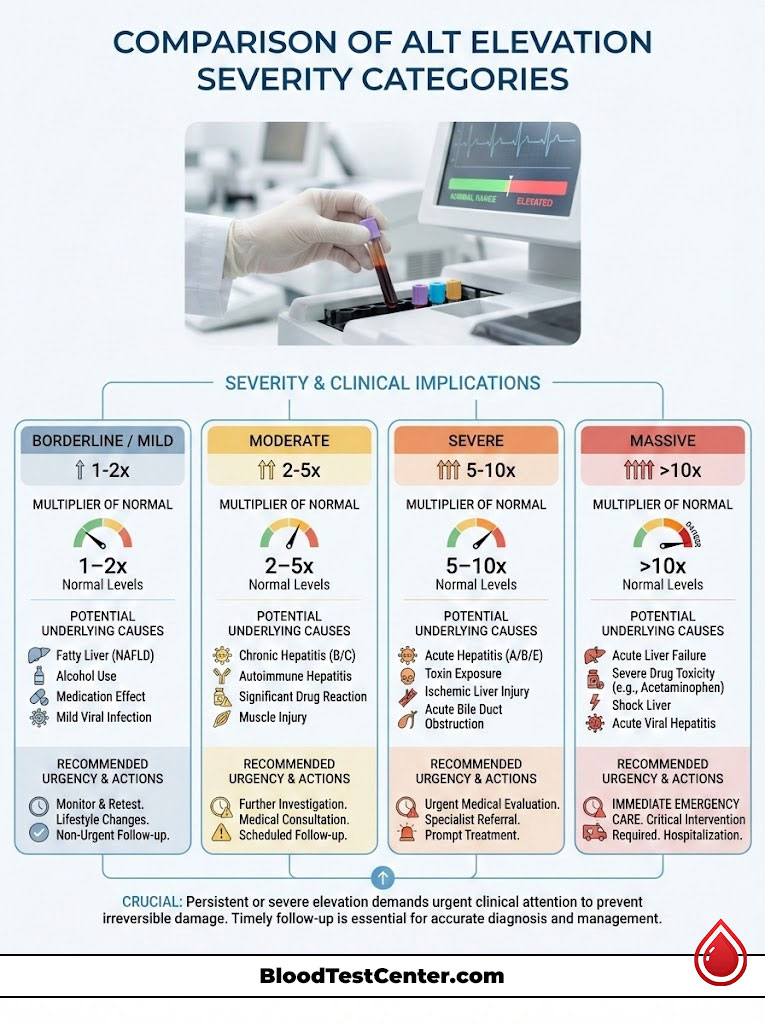
| Elevation Category | Multiplier of Normal | Potential Underlying Causes | Urgency & Action |
| Borderline / Mild | 1x – 2x Upper Limit | Fatty Liver (NAFLD), Medication effect, Alcohol, Intense Exercise | Routine Follow-up: Repeat test in 4-8 weeks. Review diet/meds. |
| Moderate | 5x – 15x Upper Limit | Chronic Viral Hepatitis, Alcoholic Liver Disease, Drug Toxicity | Prompt Evaluation: Hepatic Function Panel, Ultrasound, Viral Screening needed. |
| Severe | >15x Upper Limit | Acute Hepatitis (A, B, C), Tylenol Overdose, Ischemic Liver Injury | Immediate Attention: Urgent medical intervention required to prevent failure. |
| Massive | >50x Upper Limit | Shock Liver, Acute Toxin Ingestion | Emergency: Critical care usually required. |
Common Causes of Elevated ALT in a Routine Metabolic Panel
When an otherwise healthy adult presents with high liver enzymes during a physical, the differential diagnosis in the USA usually points to four main categories. Physicians work through these possibilities systematically.
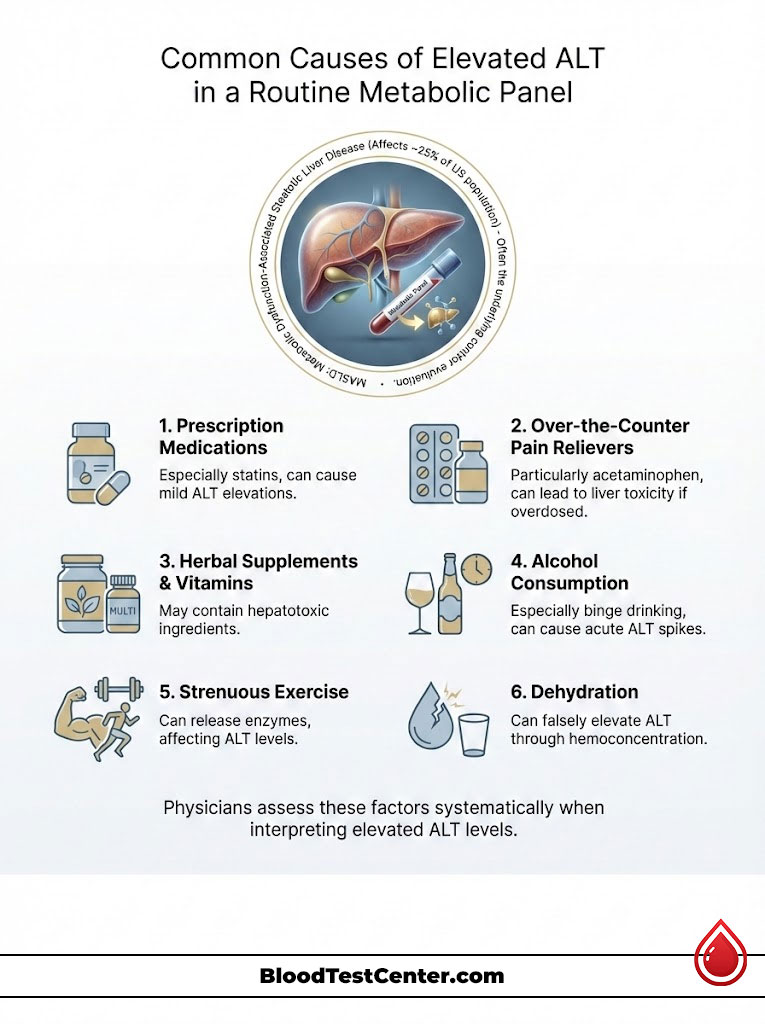
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD)
The most prevalent cause of an elevated ALT in a routine panel in America is Non-Alcoholic Fatty Liver Disease (NAFLD), which has recently been renamed Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) to better reflect its cause.
This condition affects nearly 25% of the US population. It occurs when excess fat is stored in liver cells, unrelated to alcohol use. This visceral fat is not inert. It is toxic to the cells (lipotoxicity), causing chronic inflammation and low-level enzyme leakage. If your CMP blood test also shows high fasting glucose, high triglycerides, or if you carry excess weight around the abdomen, NAFLD is the primary suspect. It is the hepatic manifestation of metabolic syndrome.
Impact of Prescription Medications and Statins on Liver Enzymes
Your liver is the body’s primary filtration and detoxification system. Almost every medication you swallow must be metabolized by the liver before it can leave your body. This workload can sometimes cause stress.
Statins (cholesterol-lowering drugs like Atorvastatin or Rosuvastatin) are known to cause mild, asymptomatic elevations in Alanine Aminotransferase. In most cases, this is a phenomenon known as “transaminitis” and is not dangerous. It often resolves on its own or stabilizes. Physicians rarely stop these life-saving heart medications unless the liver enzymes rise to more than three times the upper limit of normal.
Antibiotics, anti-seizure medications, and even acne treatments like isotretinoin can also trigger temporary elevations.
Risks of Over-the-Counter Pain Relievers and Acetaminophen Toxicity
One of the most overlooked causes comes from the pharmacy aisle. Acetaminophen (the active ingredient in Tylenol and many cold/flu remedies) is safe at recommended doses but can be potent liver toxin if taken in excess.
Because Acetaminophen is found in so many different products (sleep aids, cough syrups, pain pills), it is easy to accidentally “stack” doses. Even taking the maximum daily dose for a few days to treat a stubborn flu can cause a temporary, sharp spike in ALT. This is often the culprit when a patient sees a surprisingly high number after being sick the week prior.
Hidden Dangers in Herbal Supplements and Vitamins
Many Americans operate under the assumption that “natural” means safe. However, the supplement industry is not regulated as strictly as pharmaceuticals, and many herbs are processed by the liver.
Supplements such as Green Tea Extract (often found in weight loss pills), Kava Kava (used for anxiety), and certain bodybuilding pre-workout formulas can be hepatotoxic (toxic to the liver). High doses of Vitamin A are also a known cause of liver stress. A thorough doctor will ask about every pill, powder, or tea you consume, not just prescription drugs.
Alcohol Consumption and Acute Enzyme Spikes
Alcohol is directly toxic to hepatocytes. While we often associate liver function test abnormalities with chronic alcoholism, the liver is sensitive to acute intake as well.
“Binge” drinking—defined as 4 or more drinks for women and 5 or more for men in two hours—can cause a temporary inflammatory response. If you attended a wedding or party and drank heavily 24 to 48 hours before your blood draw, your ALT might be falsely elevated. This does not necessarily mean you have alcoholic liver disease, but it does mean your liver was actively working to clear the toxin when the blood was drawn.
Transient Factors: Strenuous Exercise and Dehydration Effects
Sometimes, a high number is just a physiological glitch rather than a disease.
Strenuous physical exertion, particularly heavy weightlifting or endurance running, causes muscle micro-tears. While this is how you build strength, it releases enzymes into the bloodstream. Because ALT can exist in small amounts in muscle tissue, and because intense exercise changes total body chemistry, a heavy gym session the day before a test can skew results. Additionally, severe dehydration can cause hemoconcentration, making all the solids in your blood (including enzymes) appear more concentrated and higher than they truly are.
Using the AST to ALT Ratio (De Ritis Ratio) for Diagnosis
Physicians do not look at ALT in a vacuum. To get a clearer picture without invasive biopsies, they compare it to its partner, AST. This mathematical relationship is called the AST/ALT ratio, or historically, the De Ritis Ratio. This simple division problem gives powerful clues about the source of the damage.
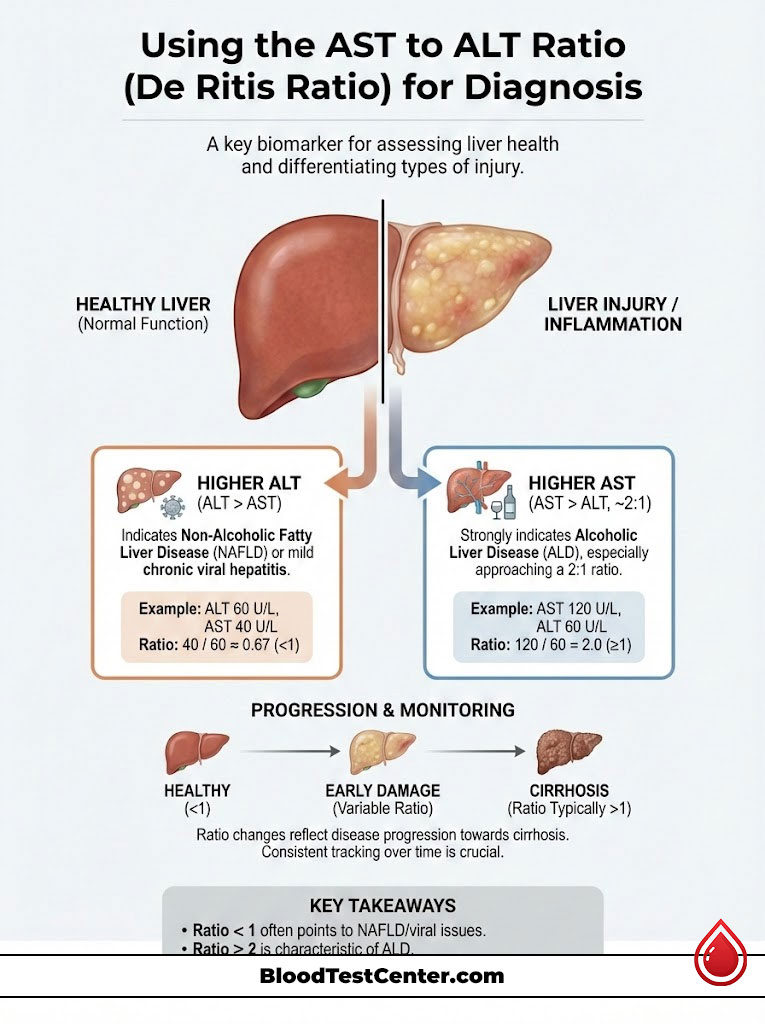
Interpreting a Ratio Where ALT is Higher Than AST
In the vast majority of Non-Alcoholic Fatty Liver Disease (NAFLD) cases and mild chronic viral hepatitis, the ALT will be higher than the AST.
For example, if your ALT is 50 and your AST is 30, the ratio is 0.6. This “less than 1” pattern is the classic signature of metabolic liver stress found in routine screenings. It suggests the inflammation is driven by fat accumulation or mild viral activity rather than alcohol or muscle trauma.
Significance of an AST Level Higher Than ALT
If the AST is significantly higher than the ALT, specifically approaching a 2:1 ratio, it strongly suggests Alcoholic Liver Disease. Alcohol specifically damages the mitochondria of the cells, which releases more AST than ALT.
Furthermore, as liver disease progresses toward cirrhosis (scarring), the ratio often flips. A liver that is becoming fibrotic may start showing higher AST levels. Therefore, a doctor monitors this ratio closely over time to track disease progression.
Comparison Table: ALT vs. AST Specifics
Understanding the distinct differences between these two enzymes helps clarify why ALT is the gold standard for liver specificity in a routine panel.
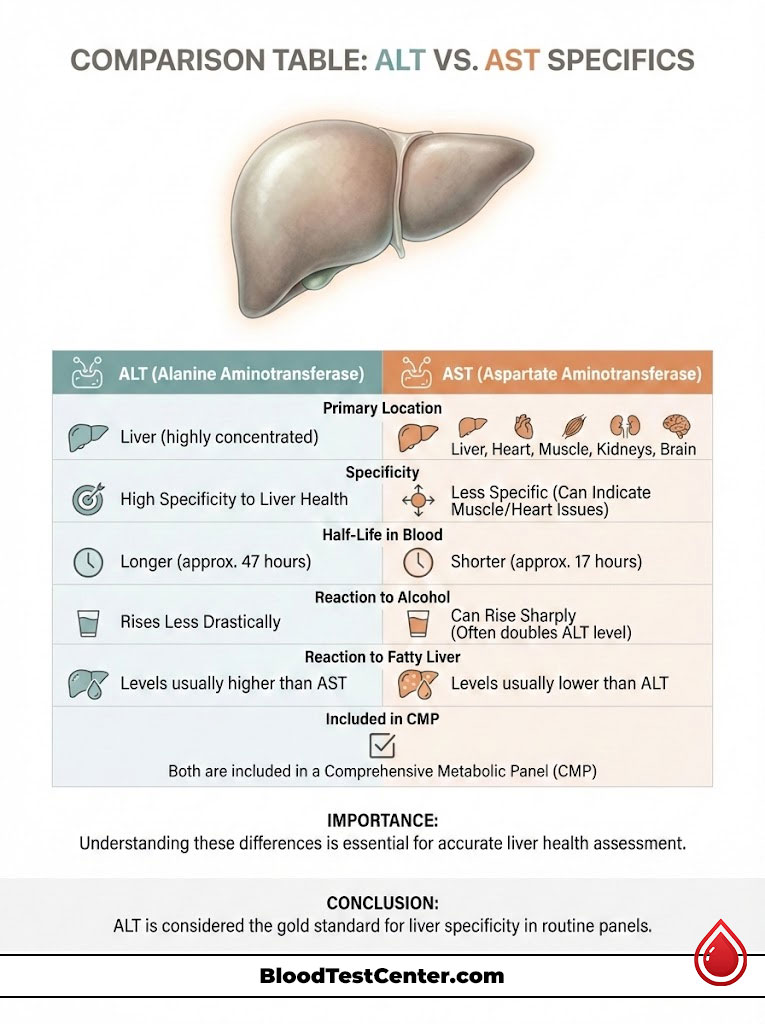
| Feature | ALT (Alanine Aminotransferase) | AST (Aspartate Aminotransferase) |
| Primary Location | Liver (Cytoplasm of cells) | Liver, Heart, Skeletal Muscle, Kidneys, Brain |
| Specificity | High (Specific to Liver health) | Low (Can indicate muscle damage or heart issues) |
| Half-Life in Blood | Longer (Approx. 47 hours) | Shorter (Approx. 17 hours) |
| Reaction to Alcohol | Rises less drastically than AST | Rises sharply (often double the ALT) |
| Reaction to Fatty Liver | Usually higher than AST | Usually lower than ALT |
| Included in CMP? | Yes | Yes |
Diagnostic Follow-Up Steps After a High ALT Result
Receiving a high result on your CMP blood test triggers a standardized clinical workflow. Doctors follow a decision tree to rule out the most dangerous causes first.
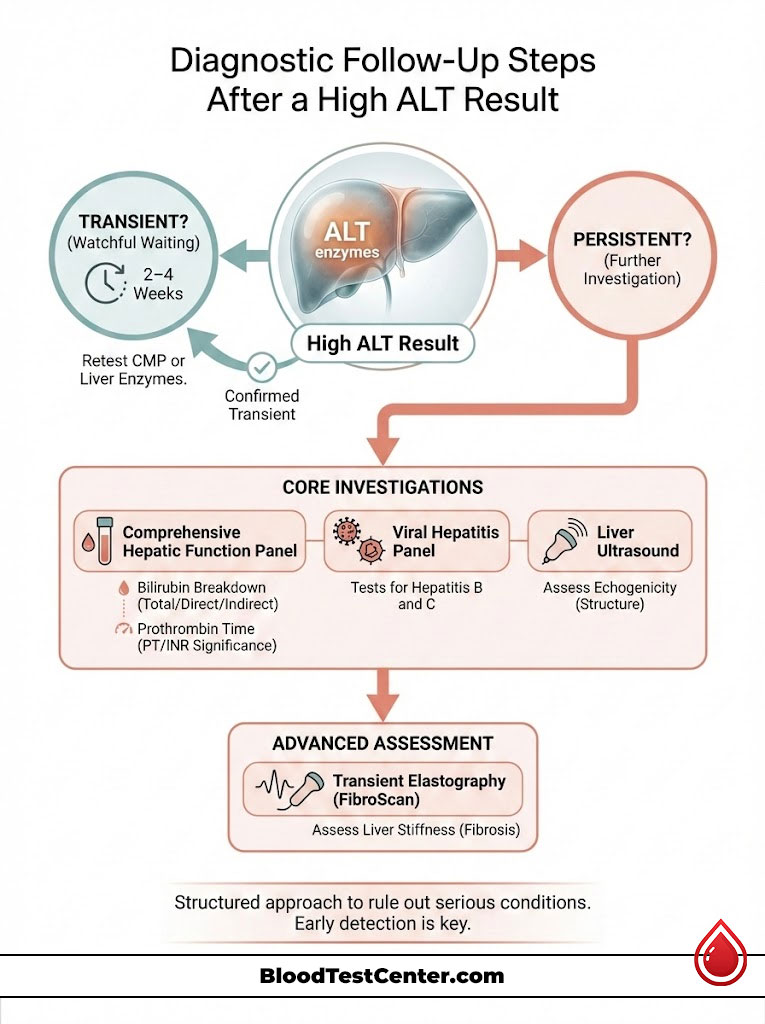
The Importance of Repeat Testing to Rule Out Transience
Because transient factors like dehydration, a recent viral cold, or a gym session can skew results, the first step is often “watchful waiting.” Guidelines typically recommend repeating the Comprehensive Metabolic Panel or just the liver enzymes in 2 to 4 weeks.
This confirms if the elevation is persistent (chronic) or if it was a one-time spike (acute/transient). Nearly 30% of mild elevations resolve on their own upon retesting without any intervention.
Comprehensive Hepatic Function Panel and Viral Screening
If the elevation persists in the second test, the doctor will order a “Hepatic Function Panel.” This is a more granular test than the general CMP.
It breaks down Bilirubin into “Direct” (conjugated) and “Indirect” (unconjugated) types. It also measures Prothrombin Time (PT/INR), which tells the doctor how fast your blood clots. This is a true measure of liver function, because the liver manufactures clotting factors. If the enzymes are high but the clotting time is normal, the liver is stressed but still functioning well.
Simultaneously, the doctor will likely order a viral hepatitis panel. This simple blood draw checks for Hepatitis B surface antigens and Hepatitis C antibodies. Hepatitis C was a “silent” epidemic for the Baby Boomer generation, and many individuals remain undiagnosed until a routine ALT check catches it.
Utilizing Liver Ultrasound and Elastography for Imaging
If blood work confirms chronic inflammation and viral causes are ruled out, the next step is usually imaging. A liver ultrasound is the standard first-line tool.
This non-invasive scan looks for “echogenicity.” If the liver looks brighter than the kidneys on the ultrasound screen, it indicates fat accumulation, confirming NAFLD. For more advanced assessment, doctors may use Transient Elastography (FibroScan). This specialized ultrasound sends a vibration wave through the liver to measure stiffness. It can instantly tell the doctor if there is scarring (fibrosis) without the need for a painful needle biopsy.
Actionable Strategies to Lower Elevated ALT Levels Naturally
If your elevated ALT in a routine panel is linked to metabolic health, diet, or lifestyle (which is true for the majority of US cases), the outlook is generally positive. The liver is the only organ in the human body capable of true regeneration.

Dietary Interventions: Reducing Fructose and Processed Carbs
The liver processes carbohydrates, specifically fructose, differently than other cells. High intake of high-fructose corn syrup (found in sodas, juices, and processed foods) drives a process called “de novo lipogenesis,” where the liver turns sugar directly into fat.
Cutting out sugary beverages and reducing processed white carbohydrates (bread, pasta) is the single most effective intervention for lowering liver enzymes. Adopting a Mediterranean Diet, rich in Omega-3 fatty acids, olive oil, vegetables, and lean proteins, has been clinically proven to reduce liver fat and inflammation.
The Protective Benefits of Coffee on Liver Enzyme Levels
Multiple large-scale epidemiological studies have confirmed a surprising ally in liver health: Coffee.
Regular coffee consumption (specifically black coffee, without heavy sugar or cream) has been consistently linked to lower liver enzyme levels and a reduced risk of fibrosis. The polyphenols and caffeine in coffee appear to downregulate inflammatory pathways (like TGF-beta) that lead to scarring. Drinking 2 to 3 cups per day is often recommended by hepatologists as a therapeutic adjunct.
Weight Management and Its Direct Impact on Hepatocytes
You do not need to reach a “perfect” BMI to fix your labs. Clinical data shows that losing just 5% to 10% of your total body weight is sufficient to mobilize dangerous visceral fat out of the liver.
When you lose weight, the fat inside the liver is often some of the first to be burned for energy. This reduction in intra-hepatic fat relieves the stress on the cell walls, stopping the leakage of ALT. Patients often see their numbers return to the normal range within 3 to 6 months of consistent lifestyle changes.
Summary & Key Takeaways
Finding an elevated ALT in a routine panel serves as a vital “check engine light” for your body. It is a signal to pause and evaluate your metabolic health.
- Context is Everything: A high ALT in a CMP blood test indicates inflammation or cellular stress, but it is rarely an immediate emergency if found in an asymptomatic person.
- Trend Over Time: One high reading is less important than a persistent elevation. Re-testing is the standard of care to rule out temporary spikes from exercise or viruses.
- Metabolic Driver: In the USA, the vast majority of these cases are driven by NAFLD (Fatty Liver) linked to insulin resistance and weight.
- Specificity: Alanine Aminotransferase is the most specific marker for liver health. Comparing it to AST helps refine the diagnosis.
- Reversibility: The liver is resilient. Lifestyle interventions involving diet, weight loss, and avoiding toxins like excessive alcohol or unnecessary supplements can often fully reverse mild elevations.
By understanding these numbers, you transform a source of medical anxiety into a clear, actionable roadmap for long-term longevity.
Frequently Asked Questions (FAQ)
What level of ALT is considered dangerously high?
While “danger” depends on the clinical context, levels greater than 15 to 20 times the upper limit of normal (usually over 500-1000 U/L) are considered severe. This magnitude of elevation suggests acute hepatocellular injury, such as viral hepatitis, toxin ingestion, or ischemic injury, and requires immediate medical evaluation.
Can stress cause elevated ALT levels?
Psychological stress alone does not typically cause a significant spike in liver enzymes. However, severe physiological stress on the body—such as major surgery, severe burns, or trauma—can cause systemic inflammation and oxidative stress that may result in a temporary rise in ALT.
How long does it take for ALT levels to return to normal?
This timeline varies based on the underlying cause. If the elevation is due to a specific medication or an acute alcohol binge, levels often drop within weeks of stopping the substance. For metabolic conditions like NAFLD, normalization is a slower process, often taking 3 to 6 months of consistent weight loss and dietary improvement.
Should I stop taking my statins if my ALT is high?
You should never stop prescription medication without a doctor’s order. Mild liver enzyme elevations are a known, often acceptable side effect of statin therapy. Physicians generally only discontinue the drug if levels reach more than 3 times the upper limit of normal.
Does fasting affect ALT results in a CMP?
ALT itself is not significantly affected by recent food intake. However, the Comprehensive Metabolic Panel requires fasting (typically 8-12 hours) to ensure accurate readings for Glucose and Triglycerides. Eating before the test won’t falsely raise your ALT, but it will invalidate other parts of the panel.
Can a viral infection like the flu raise ALT?
Yes. Systemic viral infections, including Influenza and Mononucleosis (Mono), can cause temporary, mild inflammation in the liver. This often leads to a transient spike in Alanine Aminotransferase that resolves once the virus clears the body.
Is high ALT genetic?
It can be. While lifestyle is the most common cause, genetic disorders such as Hemochromatosis (iron overload), Wilson’s Disease (copper accumulation), and Alpha-1 Antitrypsin Deficiency can cause chronic liver enzyme elevation. Doctors screen for these if lifestyle changes do not fix the numbers.
What foods should I avoid if my ALT is high?
To reduce liver stress, you should avoid foods high in added sugars (especially high-fructose corn syrup), trans fats, and highly processed refined carbohydrates. Alcohol should be strictly eliminated until the cause of the elevation is identified and resolved.
Why is my ALT high but my AST is normal?
This pattern is the classic signature of early-stage Non-Alcoholic Fatty Liver Disease (NAFLD) or mild liver stress. Because ALT is more specific to the liver and located in the cytoplasm, it often leaks out earlier and in greater quantities than AST in metabolic conditions.
Can muscle soreness from the gym raise my ALT?
Yes. Intense physical exercise causes micro-trauma to muscle fibers. While AST is more abundant in muscle, ALT is also present. Severe exertion can release enough of both enzymes to cause a “false positive” concern for liver health.
Is an ALT of 60 bad?
An ALT of 60 U/L is generally considered a “mild elevation.” While it is not a medical emergency, it is above the optimal range for both men and women. It serves as a warning sign to investigate lifestyle factors, medication side effects, or metabolic health.
Do probiotics help lower ALT?
Emerging research into the “gut-liver axis” suggests that gut health plays a role in liver inflammation. Some studies indicate that specific probiotic strains may help reduce intestinal permeability (“leaky gut”) and lower endotoxins, potentially helping to reduce liver enzyme levels in patients with fatty liver.
Disclaimer
The content provided in this article is for educational and informational purposes only. It does not constitute medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider regarding your specific medical condition, medication changes, or interpretation of your laboratory results.
References
- American College of Gastroenterology (ACG). ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries.
- National Institutes of Health (NIH). LiverTox: Clinical and Research Information on Drug-Induced Liver Injury.
- Centers for Disease Control and Prevention (CDC). Viral Hepatitis Surveillance and Statistics.
- Journal of Hepatology. The role of coffee in the management of non-alcoholic fatty liver disease.
- American Association for the Study of Liver Diseases (AASLD). The Diagnosis and Management of Non-Alcoholic Fatty Liver Disease.

