When you receive your lab report after a routine blood draw, you’re often faced with a page full of medical acronyms, numbers, and ranges. While it’s easy to focus on values like cholesterol or glucose, one of the most powerful and insightful measurements on that page is a three-letter acronym: MCV.
Table of Contents
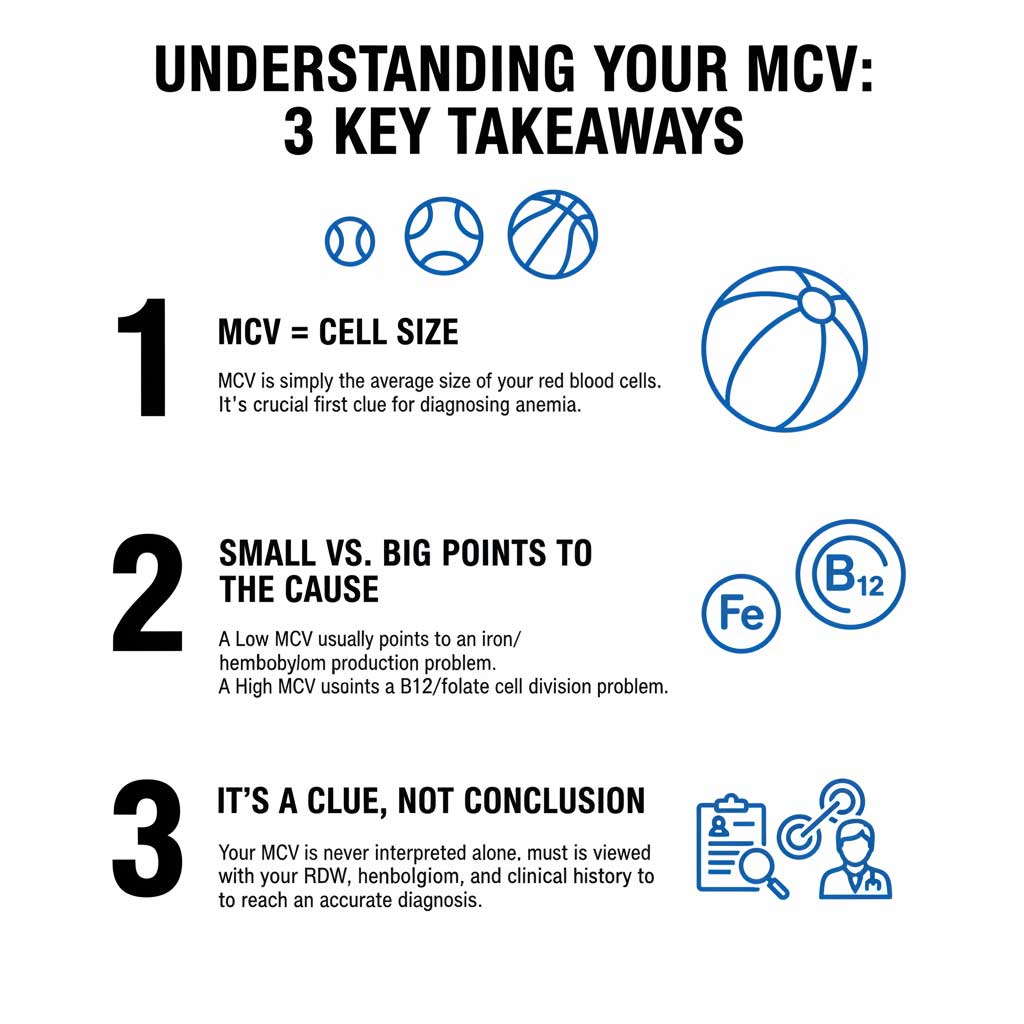
So, what is MCV in a blood test, and why do doctors pay such close attention to it? This comprehensive guide from BloodTestCenter.com will demystify the Mean Corpuscular Volume (MCV), explaining what it measures, what the normal ranges are, and what a high or low result could mean for your health. While the MCV is not a diagnosis on its own, it is arguably the single most important clue that helps your doctor classify different types of anemia and investigate a wide range of underlying health conditions—sometimes long before you even feel sick.
What Exactly is MCV? The Basics Explained
Understanding your MCV is much simpler than it sounds. It’s a key part of a standard Complete Blood Count (CBC) test, and its purpose is straightforward.
MCV Stands for Mean Corpuscular Volume
Let’s break down the term itself:
- Mean: This is just the mathematical term for “average.”
- Corpuscular: This is a scientific term related to a “corpuscle,” or a cell. In a CBC, it refers specifically to your red blood cells.
- Volume: This simply means size.
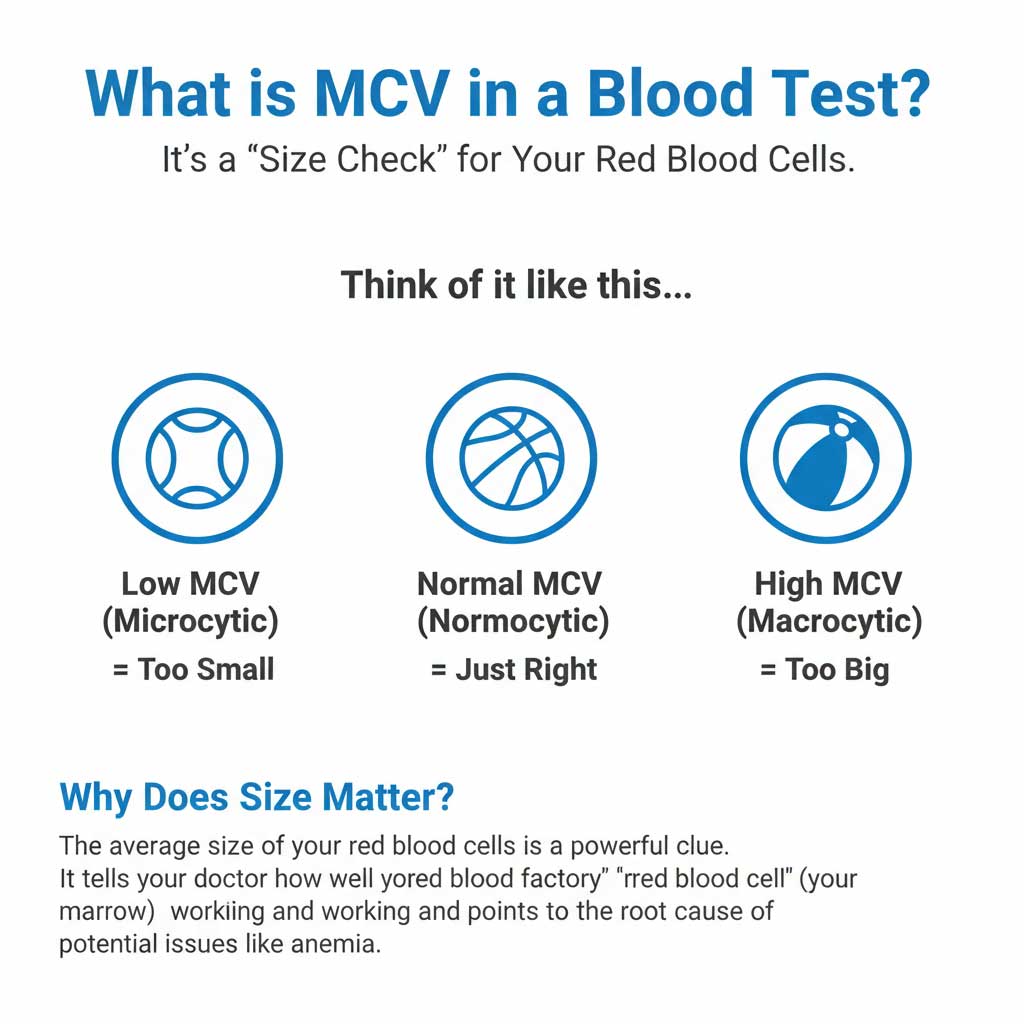
So, the Mean Corpuscular Volume is a direct measurement of the average size of your red blood cells.
Think of it like this: if you could somehow look at a million of your red blood cells, the MCV would tell you their average size. It answers the question, “On average, are my red blood cells the correct size, are they too small, or are they too big?”
Why is the Size of Red Blood Cells So Important?
Your red blood cells have one of the most critical jobs in your body: they are the delivery trucks for oxygen. They are filled with a protein called hemoglobin, which picks up oxygen in your lungs and carries it to every tissue and organ. For this system to work efficiently, your red blood cells need to be the right size and shape.
An abnormal average size is a major red flag that the “production factory” for your red blood cells—your bone marrow—is having a problem. The type of size abnormality (too big or too small) provides a powerful clue as to the type of problem the factory is facing.
How is MCV Measured?
The MCV is automatically calculated by a machine called a hematology analyzer as part of a routine CBC test. It is measured in incredibly tiny units of volume called femtoliters (fL). You can easily order a CBC test online through BloodTestCenter.com to get a precise measurement of your MCV and other crucial blood parameters.
The MCV Normal Range: What Are We Aiming For?
Like most lab tests, the MCV has a “normal” range. Results that fall within this range indicate that your red blood cells are, on average, a healthy size.
The Goldilocks Zone: 80 to 100 fL
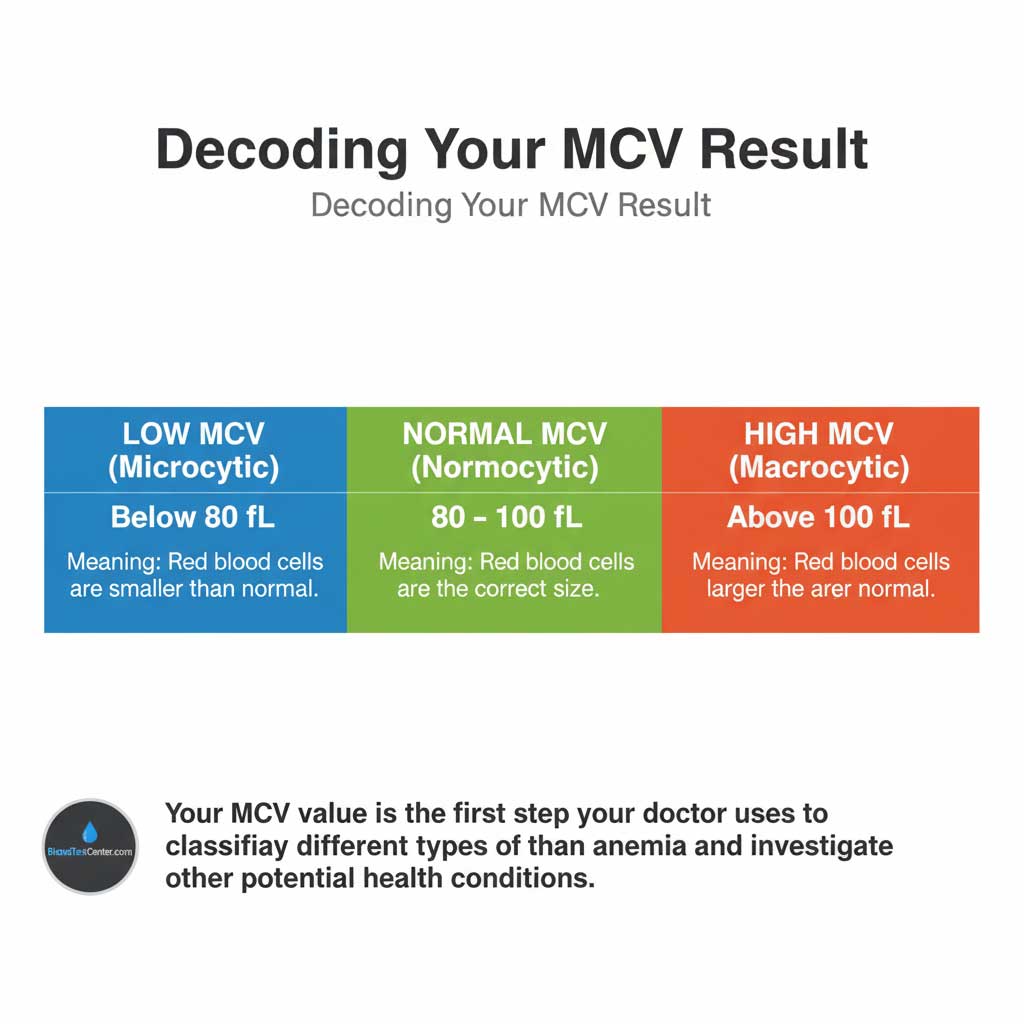
For most healthy adults in the U.S., the standard MCV normal range is 80 to 100 femtoliters. A result in this range means your red blood cells are of a normal size, a state referred to as normocytic.
Below the Range: Low MCV (Microcytosis)
A low MCV is generally defined as a value below 80 fL. This indicates that your red blood cells are, on average, smaller than normal. The medical term for this is microcytosis. If you also have low hemoglobin, this is classified as microcytic anemia.
Above the Range: High MCV (Macrocytosis)
A high MCV is generally defined as a value above 100 fL. This indicates that your red blood cells are, on average, larger than normal. The medical term for this is macrocytosis. If you also have low hemoglobin, this is classified as macrocytic anemia.
High MCV (Macrocytosis): When Your Red Blood Cells Are Too Big
Seeing a high MCV on your lab report is a significant finding that points your doctor toward a specific set of potential causes.
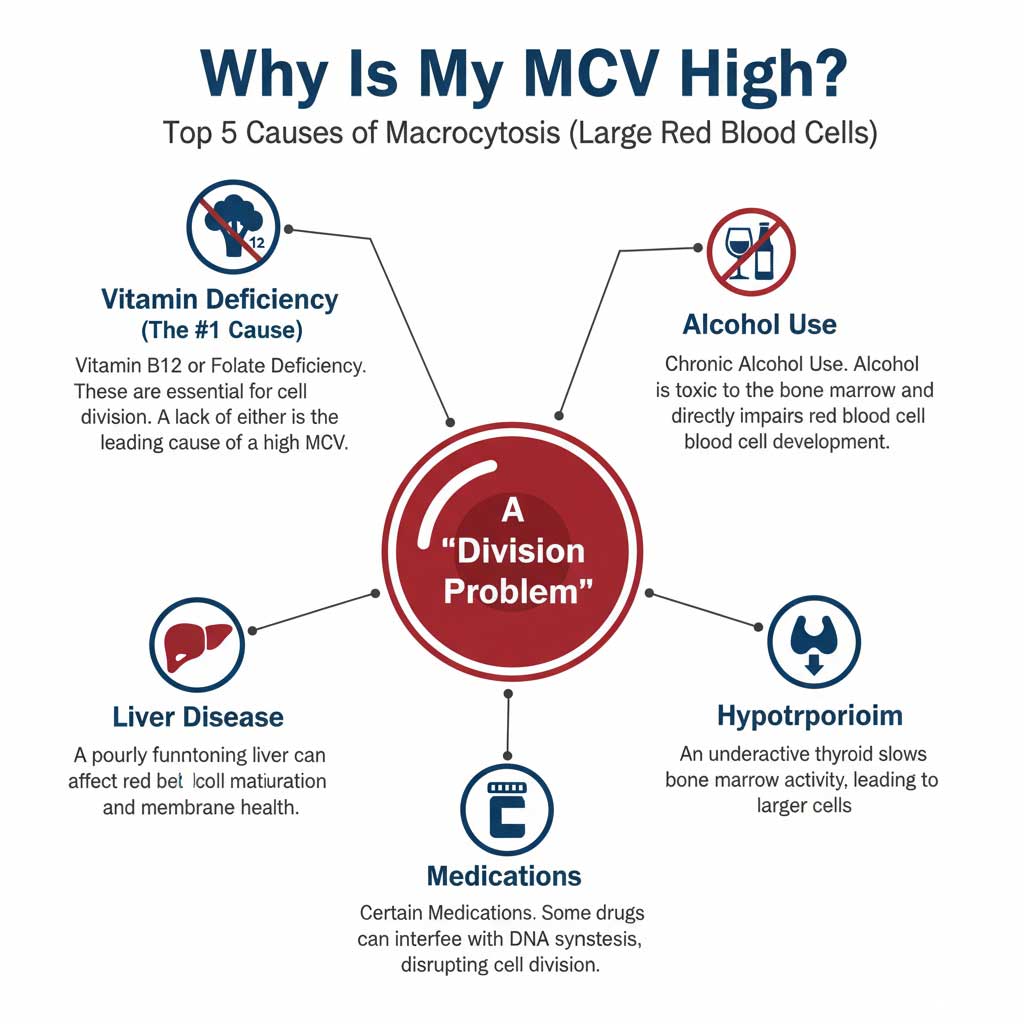
The Root Cause: A Problem with Cell Division
In most cases, a high MCV is a “division problem.” Inside your bone marrow, red blood cell precursors are supposed to grow and then divide several times before they mature and are released into your bloodstream. Certain nutrient deficiencies can interfere with this division process. The cells continue to grow, but they fail to divide properly, resulting in abnormally large, often immature red blood cells being released. This is the hallmark of macrocytic anemia.
Top Causes of a High MCV
The list of potential causes for macrocytosis is relatively short, making the MCV a very useful diagnostic tool.
- Vitamin B12 or Folate DeficiencyThis is the number one cause of a high MCV. Vitamin B12 and folate (Vitamin B9) are absolutely essential for the synthesis of DNA. Without enough of these vitamins, the bone marrow cannot produce DNA quickly enough for the rapidly dividing red blood cell precursors. This is the classic vitamin B12 deficiency MCV connection and is a prime example of how the Mean Corpuscular Volume can help detect vitamin deficiencies.
- Alcohol UseDoes alcohol consumption raise MCV? Yes, significantly. Chronic and heavy alcohol use is directly toxic to the bone marrow. It can impair the development of red blood cells and lead to a high MCV, even in the absence of a vitamin deficiency.
- Liver DiseaseThe liver plays a complex role in processing nutrients and maintaining the health of red blood cell membranes. Chronic liver disease is a well-known and common cause of a high MCV.
- HypothyroidismAn underactive thyroid gland slows down all of your body’s metabolic processes, including the rate of cell production in your bone marrow. This can lead to the production of larger red blood cells.
- Certain MedicationsSome medications, particularly certain chemotherapy agents, anticonvulsants, and drugs used to treat HIV, can interfere with DNA synthesis and cause the MCV to rise.
What if I have a High MCV but Normal Hemoglobin?
This is a very common and important clinical scenario. If you have a high MCV normal hemoglobin, it means your red blood cells are oversized, but your body is still managing to produce enough of them to keep your hemoglobin level from dropping into the anemic range—for now. This is often the earliest detectable sign of a developing vitamin B12 deficiency MCV or folate deficiency. It’s a critical warning flag that allows you to intervene with diet or supplements before full-blown macrocytic anemia develops.
Low MCV (Microcytosis): When Your Red Blood Cells Are Too Small
A low MCV on your report points your doctor in a completely different direction, typically toward issues with hemoglobin production.
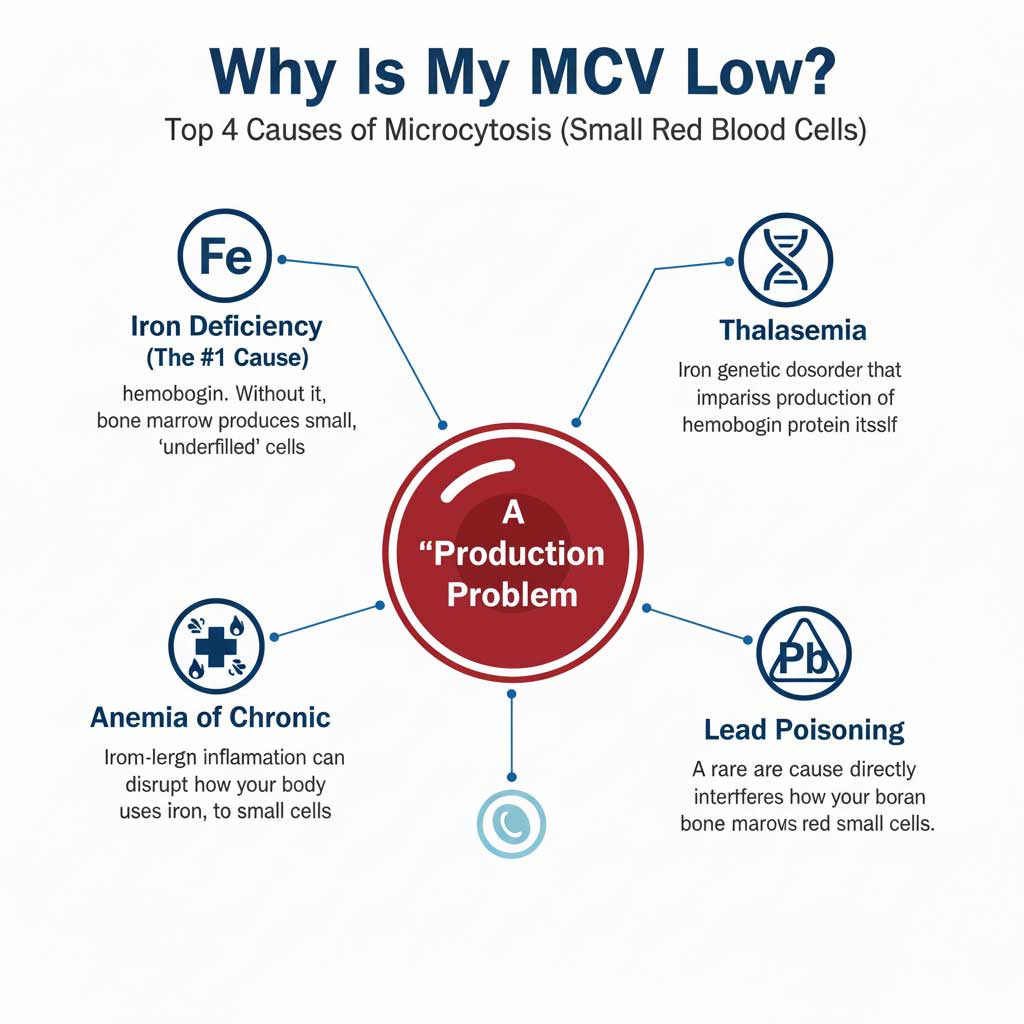
The Root Cause: A Problem with Hemoglobin Production
In most cases, a low MCV is a “production problem.” Specifically, it’s an issue with the production of hemoglobin, the iron-rich protein that fills red blood cells and gives them their color. The bone marrow’s goal is to pack each red blood cell with a sufficient amount of hemoglobin. If there isn’t enough hemoglobin available, the factory produces smaller, paler, “underfilled” cells. This results in microcytic anemia.
Top Causes of a Low MCV
- Iron Deficiency AnemiaThis is, by an overwhelming margin, the most common cause of a low MCV in the world. Iron is the central and essential building block of the hemoglobin molecule. Without enough iron, your bone marrow simply cannot produce enough hemoglobin. The link between iron deficiency anemia MCV is direct and predictable.
- ThalassemiaThis is a group of genetic blood disorders that impair the body’s ability to produce one of the globin protein chains that form the hemoglobin molecule. In individuals with thalassemia, the red blood cells are characteristically very small (a very low MCV), but their iron levels are often normal or even high.
- Anemia of Chronic Disease/InflammationLong-term inflammatory conditions, such as rheumatoid arthritis, inflammatory bowel disease, or chronic infections, can disrupt how your body absorbs and utilizes iron. This can lead to a functional iron deficiency and, consequently, a low MCV.
- Lead PoisoningA rarer cause, lead toxicity can interfere with several steps in the hemoglobin synthesis pathway, leading to a low MCV.
MCV’s Teammates: Understanding MCH, MCHC, and RDW
The MCV is a team captain, but it’s never interpreted in isolation. To get the full story, your doctor looks at it alongside a panel of other “red blood cell indices” that are also part of your CBC test results explained.
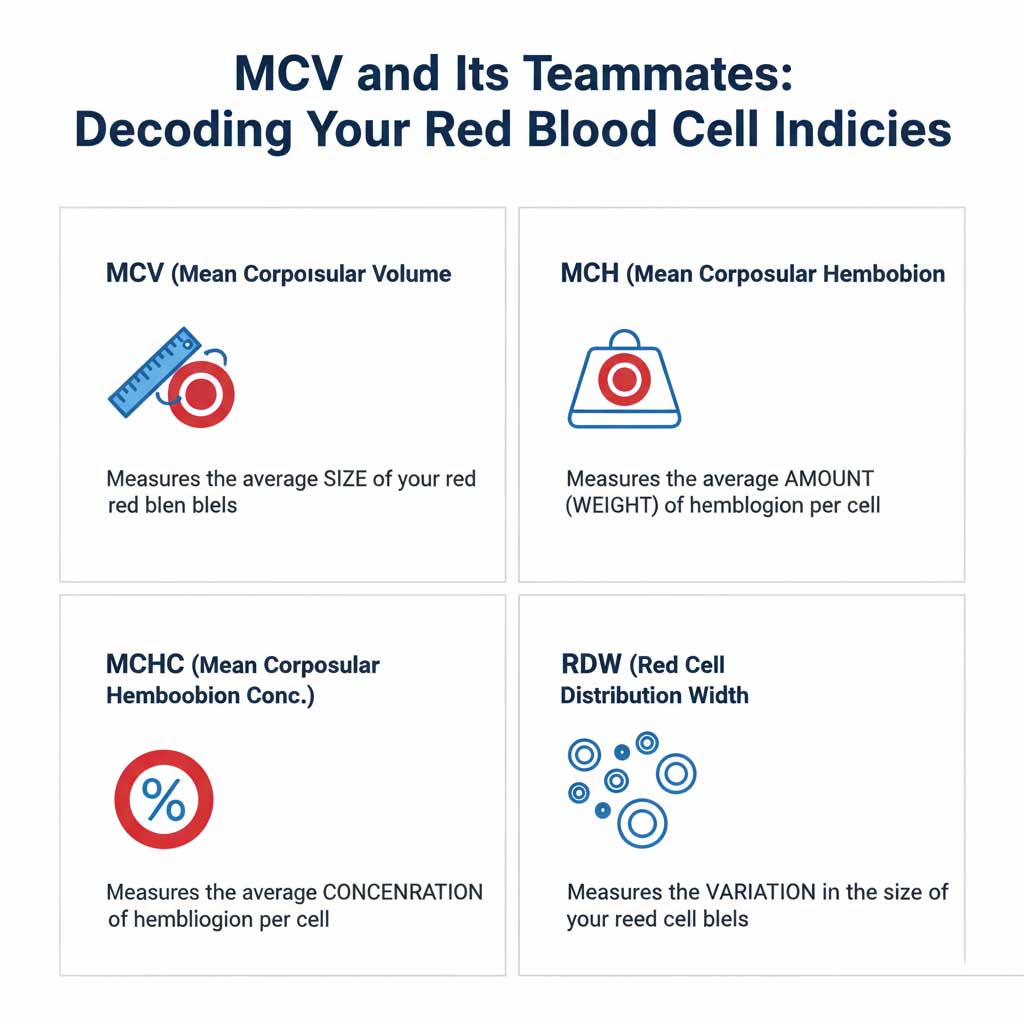
Defining the Rest of the Panel
- What is MCH in blood test? MCH stands for Mean Corpuscular Hemoglobin. It measures the average weight (amount) of hemoglobin inside a single red blood cell.
- MCHC stands for Mean Corpuscular Hemoglobin Concentration. It measures the concentration of hemoglobin in a given volume of red blood cells.
- RDW stands for Red Cell Distribution Width. This is a critically important measurement of the variation in the size of your red blood cells.
The Power of MCV and RDW Together
The combination of the MCV and RDW in blood test results is incredibly powerful for diagnosis. The RDW tells your doctor if your red blood cells are all a uniform size (normal RDW) or if there is a wide variety of sizes in circulation (high RDW).
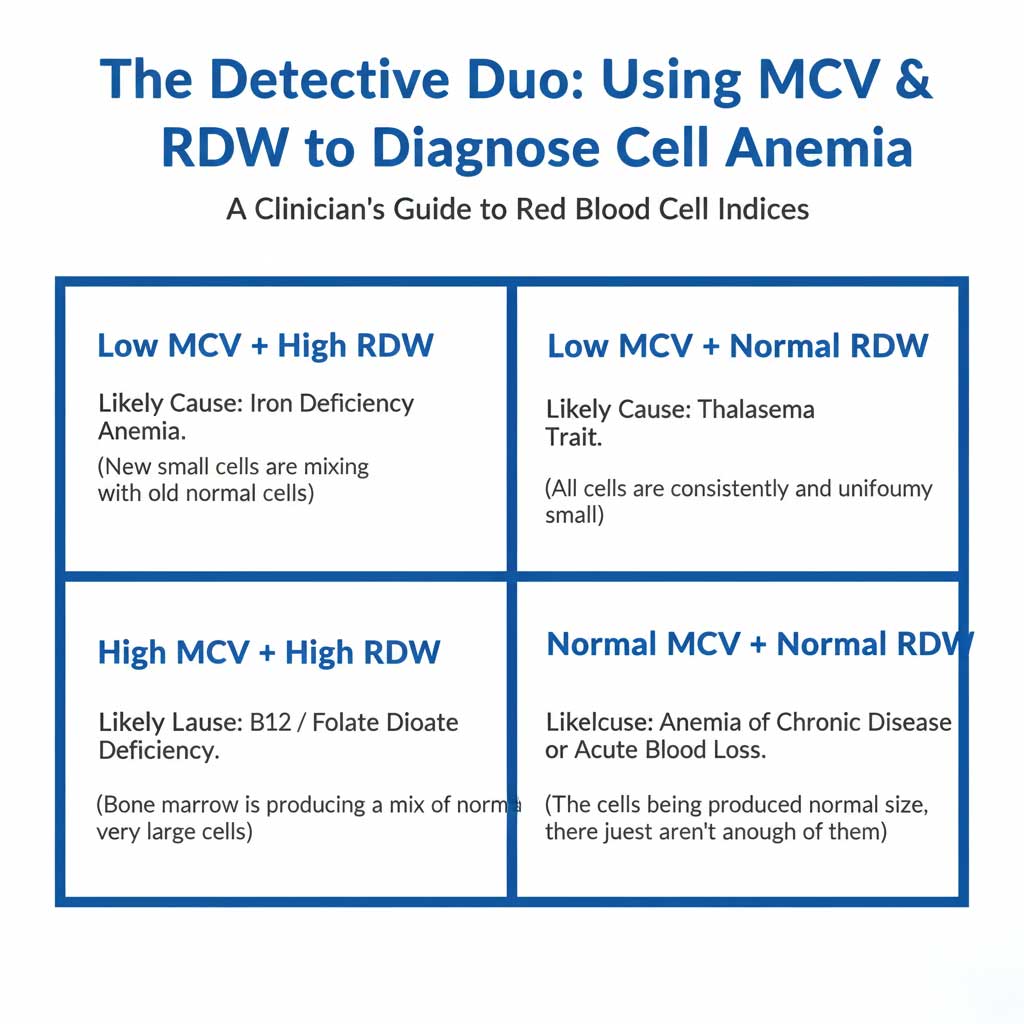
Clinical Instance: In iron deficiency anemia MCV is low, and the RDW is typically HIGH. This is because as the deficiency develops, the bone marrow starts producing new, smaller cells, which then mix with the older, normal-sized cells still in circulation. This mix of sizes drives the RDW up. In contrast, in thalassemia trait, the MCV is low, but the RDW is often NORMAL because the genetic issue causes all of the cells to be uniformly small. This is a key way doctors differentiate between the two conditions.
| Anemia Type (Classified by MCV) | MCV Result | MCH/MCHC | RDW | Common Causes |
| Microcytic Anemia | Low (<80 fL) | Low (Hypochromic) | Often High | Iron Deficiency, Thalassemia, Anemia of Chronic Disease, Lead Poisoning. |
| Normocytic Anemia | Normal (80-100 fL) | Normal (Normochromic) | Often Normal | Acute Blood Loss, Kidney Disease, Early stages of deficiency, Anemia of Chronic Disease. |
| Macrocytic Anemia | High (>100 fL) | Often High | Often High | Vitamin B12 Deficiency, Folate Deficiency, Liver Disease, Alcoholism, Hypothyroidism. |
Putting It All Together: The Diagnostic Process
When your doctor sees an abnormal MCV result, they begin a logical diagnostic process.
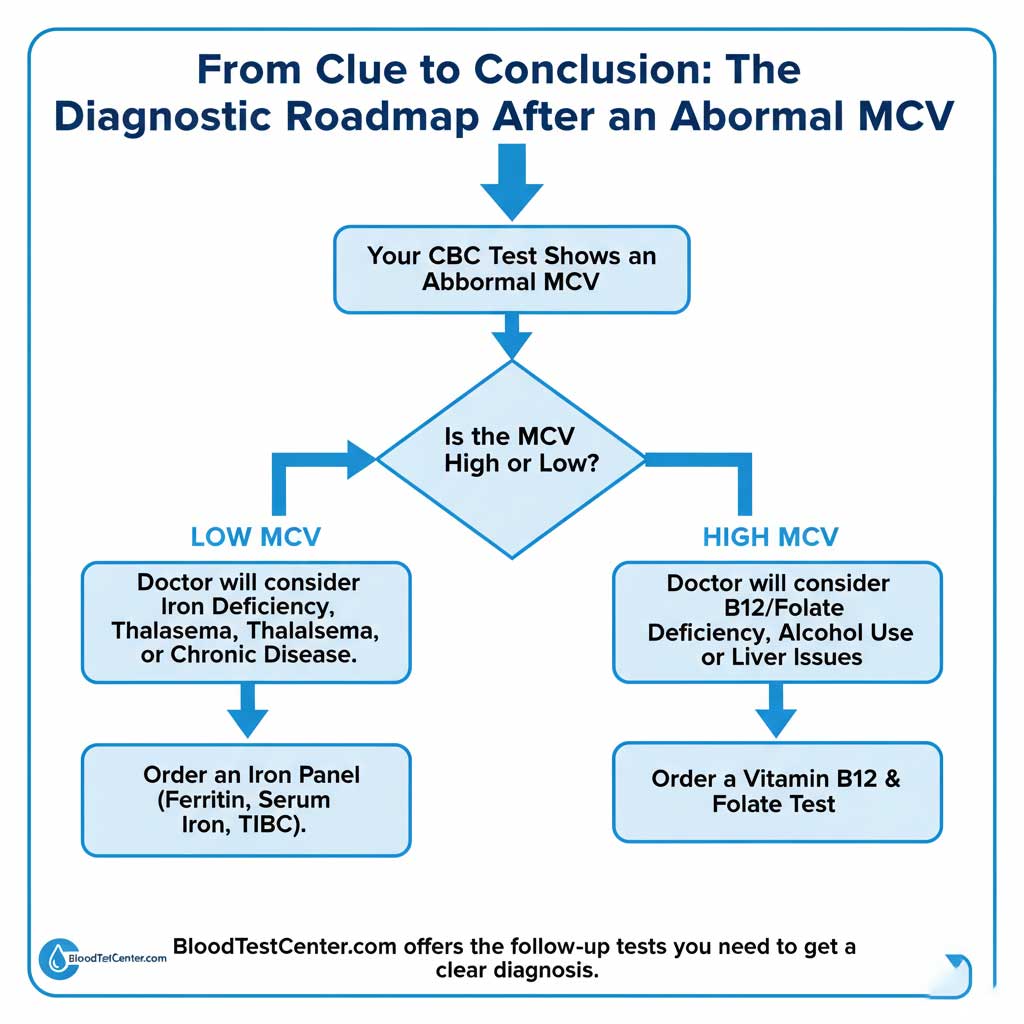
Step 1: Look at the Whole CBC Report
The first step is always to analyze the MCV in context. Is the hemoglobin low? Is the RDW high or normal? How do the MCH and MCHC look? This initial analysis, as shown in the table above, immediately narrows down the possibilities.
Step 2: Clinical History and Symptoms
Next, your doctor will correlate the lab results with you as a person. They will ask about:
- Diet: Are you on a vegan or vegetarian diet (a risk factor for B12 deficiency)?
- Lifestyle: How much alcohol do you consume?
- Symptoms: Are you experiencing fatigue, shortness of breath, or neurological symptoms like tingling in your hands and feet (a classic sign of B12 deficiency)?
Step 3: Ordering Follow-Up Tests
The CBC and your history will point toward the most likely cause, which is then confirmed with specific follow-up tests.
- If your MCV is low, the next step is almost always an Iron Panel, which includes tests for ferritin (your body’s iron stores), serum iron, and transferrin saturation.
- If your MCV is high, the next step is to order blood tests for Vitamin B12 and Folate levels.
Based on your initial CBC results, your doctor may recommend these follow-up tests. You can conveniently order an Iron Panel or a Vitamin B12 & Folate Test through BloodTestCenter.com to get these crucial answers quickly and prepare for your next appointment.
Conclusion: Your MCV is a Clue, Not a Conclusion
So, what is MCV in a blood test? It’s a precise measurement of the average size of your red blood cells, and it is one of the most useful clues in your entire lab report. It acts as a compass, pointing your doctor toward the right diagnosis. A low MCV typically indicates a problem with hemoglobin production (think iron), while a high MCV suggests a problem with cell division (think B12 and folate).
Your Mean Corpuscular Volume is a powerful, proactive health indicator. An abnormal result, even if you have high MCV normal hemoglobin, is an opportunity. It allows you and your doctor to investigate and correct an underlying nutritional deficiency or health issue before it progresses to a more serious stage.
Don’t ignore the clues hidden in your blood work. Use the CBC test results explained in this guide to have a more informed conversation with your doctor. If you need a CBC or any follow-up testing to investigate your MCV, visit BloodTestCenter.com to take the next step toward a clearer picture of your health.
Frequently Asked Questions (FAQ)
1. Is a slightly high MCV (e.g., 101 fL) dangerous?
A slightly high MCV is not dangerous in itself, but it is a significant warning sign that should not be ignored. It is often the very first indicator of an early vitamin B12 or folate deficiency, or it could be related to alcohol use. It’s a prompt for further investigation.
2. How can I lower my high MCV naturally?
You can how to lower high MCV by addressing the root cause. If it’s due to a vitamin deficiency, treatment with B12 or folate supplements will normalize the MCV over time. If it’s caused by alcohol, reducing or eliminating alcohol consumption will allow the bone marrow to recover and produce normal-sized cells.
3. How long does it take for MCV to normalize after starting treatment?
Red blood cells have a lifespan of about 120 days. Therefore, it takes several months for the older, abnormal cells to be replaced by new, healthy ones. You may start to see a trend toward normalization within a few weeks, but it can take 3 to 6 months for the MCV to fully return to the normal range.
4. Can dehydration affect my MCV result?
Severe dehydration can cause many lab abnormalities, but it does not typically have a direct, significant impact on the MCV itself, which is a measurement of the average cell size.
5. What does it mean if my MCV and MCH are both high?
A high MCV (large cells) and a high MCH (more hemoglobin per cell) almost always go together. Because the cells are larger, they can physically hold a greater amount of hemoglobin. The causes are the same as for a high MCV alone: B12/folate deficiency, liver disease, or alcohol use.
6. Can my MCV be low without me being anemic?
Yes. You can have a low MCV with a normal hemoglobin level. This is often the case in thalassemia trait, a genetic condition where the red blood cells are naturally small but are produced in sufficient numbers to prevent anemia. It can also be an early sign of developing iron deficiency.
7. Does pregnancy change the normal MCV range?
Yes. During pregnancy, a woman’s blood volume increases, and there can be a slight increase in the MCV. This is generally a normal physiological change.
8. Can I have a vitamin B12 deficiency even if my MCV is normal?
Yes. While a high MCV is a classic sign, a significant number of people with a proven B12 deficiency (especially older adults) can have a normal MCV. This can happen if they also have a co-existing condition that lowers the MCV, like iron deficiency, which “averages out” the cell size. Neurological symptoms of B12 deficiency can also occur before the MCV becomes elevated.
9. Is there a normal MCV range chart by age for children?
Yes, the MCV normal range is different for newborns, infants, and children, and it changes as they grow. Newborns have a very high MCV, which gradually decreases throughout childhood until it reaches the adult range in the late teen years.
10. Can stress cause a high or low MCV?
No, acute or chronic psychological stress does not have a direct effect on the physical size of your red blood cells. The MCV is affected by nutritional, genetic, and specific medical conditions, not by stress hormones