There is a distinct moment of anxiety that occurs when you log into your patient portal or open a lab envelope and see a number highlighted in bold red ink. Blood test results can feel like a foreign language. Among the many metrics listed on a Complete Blood Count (CBC) panel, the platelet count is one of the most critical indicators of your immediate health and vascular safety. It tells a story about your bone marrow function, your immune system, and your body’s ability to protect itself from bleeding.
Table of Contents
A normal platelet count generally falls between 150,000 and 450,000 platelets per microliter (mcL) of blood.
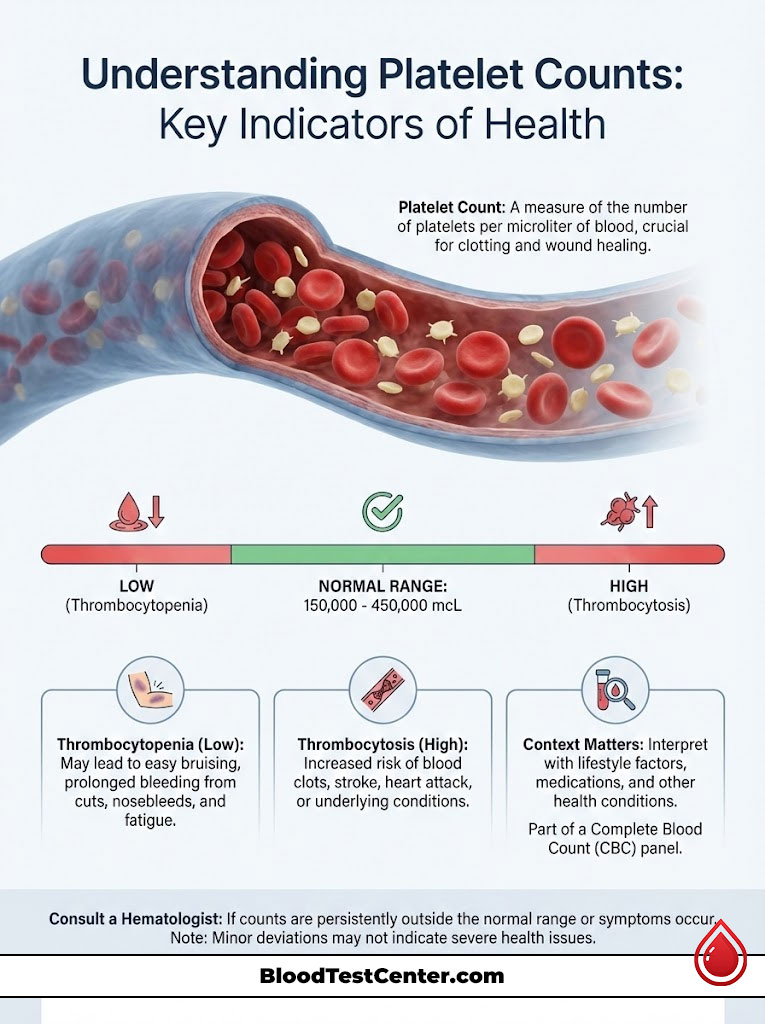
If your results show a number lower than 150,000, you are experiencing a condition medically known as thrombocytopenia (low platelet count). Conversely, if your count exceeds 450,000, you have thrombocytosis (high platelet count). While these medical terms can sound alarming, the numbers exist on a spectrum. A result slightly outside the standard reference range often points to minor lifestyle factors rather than a catastrophic illness. This guide provides a comprehensive, deep-dive analysis into what these numbers actually mean for your health, how to interpret “borderline” results, and when a hematologist should intervene.
Understanding the Role of Platelets in Human Physiology
To understand why your platelet count matters, we must first look at the microscopic “first responders” circulating in your veins. Platelets, or thrombocytes, are not actually complete cells. They are small, colorless cell fragments.
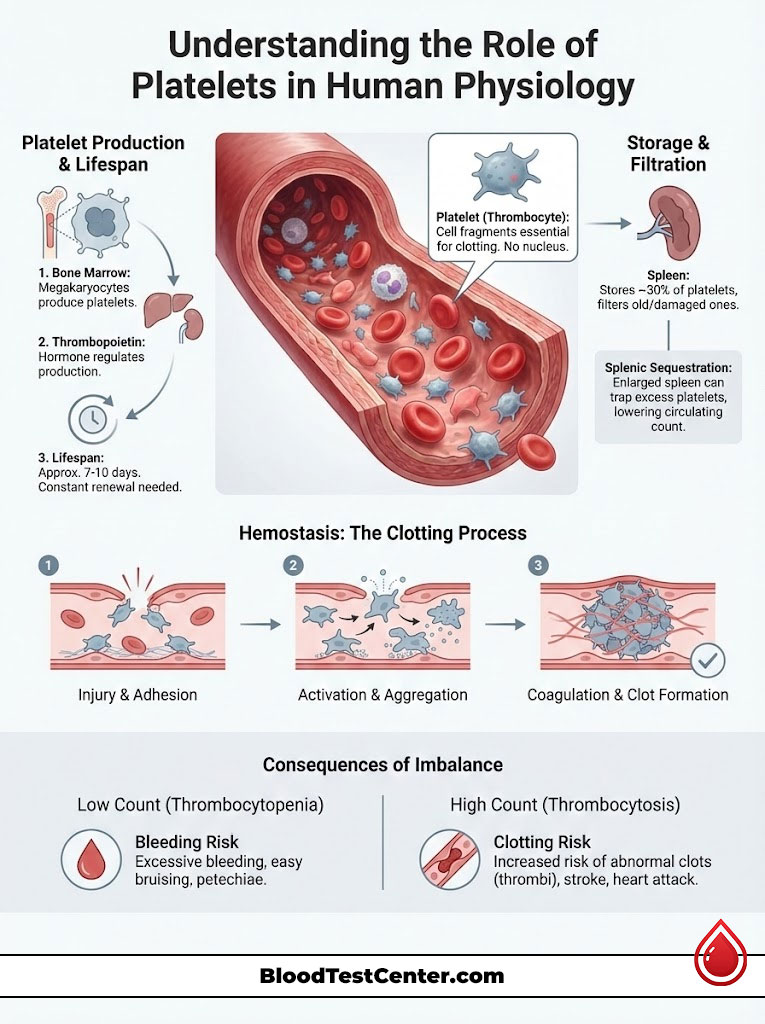
How Bone Marrow Produces Platelets
The lifecycle of a platelet begins in the spongy tissue inside your bones known as bone marrow. Here, giant cells called megakaryocytes undergo a complex process of fragmentation. One single megakaryocyte can shed thousands of platelets into the bloodstream. This production line is controlled by a hormone called thrombopoietin, which is primarily produced by the liver.
Because platelets only live for about 7 to 10 days in the human body, your bone marrow must be in a constant state of production. It must generate billions of new platelets daily to maintain a normal platelet count range. If the marrow is suppressed by a viral infection, chemotherapy, or an alcohol-induced toxicity, production slows down, leading to a rapid drop in circulating levels.
The Function of the Spleen and Sequestration
Your spleen acts as a blood filter and a storage unit for your immune system. In a healthy adult, about one-third of the body’s total platelets are stored in the spleen at any given time, ready to be deployed if an injury occurs.
However, if the spleen becomes enlarged due to liver disease or infection (a condition called splenomegaly), it can trap too many platelets. This is known as splenic sequestration. In this scenario, your bone marrow might be producing enough cells, but they are getting stuck in the spleen. This results in a low platelet count on your blood test, even though your body technically has enough platelets produced. This distinction is vital for doctors when diagnosing the root cause of abnormal platelet levels.
Hemostasis: The Clotting Process
The primary function of platelets is hemostasis. This is the body’s mechanism to stop bleeding. When a blood vessel is damaged, it sends out chemical signals. Platelets rush to the site and undergo a shape change. They sprout “sticky” tentacles and adhere to the vessel wall and to each other. This forms a temporary “platelet plug.”
If your platelet count is too low, this plug cannot form effectively, leading to prolonged bleeding from minor cuts. If the count is too high, platelets may stick together spontaneously, forming dangerous clots inside vessels that block blood flow to the heart or brain.
Detailed Reference Ranges: What is Normal?
While the standard benchmark is 150,000 to 450,000/mcL, “normal” can be subjective based on age, gender, and even altitude. Laboratories may have slight variations in their reference intervals, but the National Heart, Lung, and Blood Institute (NHLBI) maintains the standard guidelines used by most US clinicians.
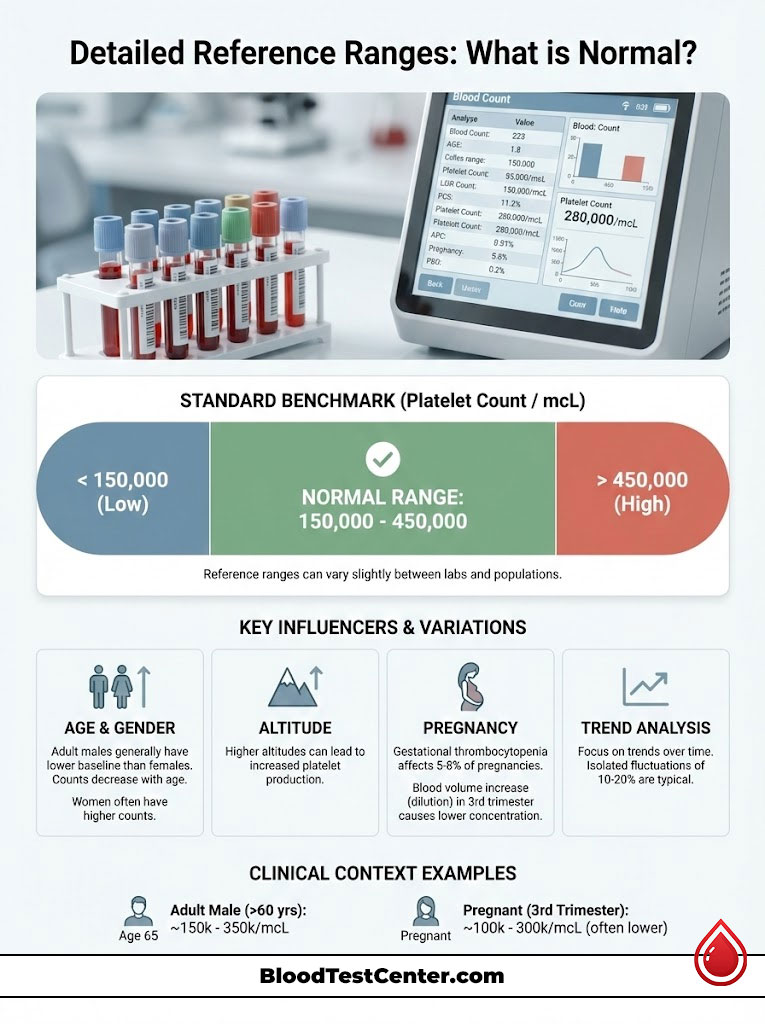
Standard Adult Platelet Count Ranges
For the vast majority of adults, staying within the standard window indicates healthy marrow function. It is important to note that a count of 145,000 or 455,000 is usually not a cause for panic. Doctors look for trends rather than single isolated numbers. Fluctuations of 10% to 20% are common day-to-day.
Platelet Counts by Age and Gender
Biological sex and age play a subtle but statistically significant role in your results. Research indicates that women often have slightly higher baseline platelet counts than men. Additionally, counts can trend downward as we age.
- Newborns and Infants: often have counts similar to adults, but premature infants may have lower thresholds that require monitoring.
- Children: typically maintain the standard high-end of the normal range due to active immune systems.
- Geriatric Populations: A natural, gradual decline in bone marrow efficiency can lead to counts settling in the lower end of the normal spectrum (e.g., 150,000 to 200,000).
Pregnancy and Gestational Thrombocytopenia
Pregnancy introduces a unique variable. During the third trimester, a woman’s blood volume increases significantly to support the baby. This leads to a dilution effect. The absolute number of platelets might be the same, but because there is more plasma (liquid), the concentration per microliter drops.
This condition is called gestational thrombocytopenia. It affects roughly 5% to 8% of pregnancies in the USA. It is usually benign and resolves on its own after delivery. However, obstetricians monitor this closely because a platelet count below 70,000 or 80,000 may prevent a woman from being eligible for an epidural during labor, as the risk of bleeding around the spine becomes too high.
| Demographic Group | Lower Limit (per mcL) | Upper Limit (per mcL) | Clinical Notes |
| Adult Males | 135,000 | 317,000 | Often slightly lower baseline than females. |
| Adult Females | 157,000 | 371,000 | Can fluctuate during menstruation. |
| Children (1-18) | 150,000 | 450,000 | Immune activity keeps counts robust. |
| Newborns | 150,000 | 350,000 | Preemies may have lower variance. |
| Pregnancy (3rd Tri) | 100,000 | 300,000 | Dilutional effect is common and usually benign. |
(Note: The ranges in this table are approximate clinical averages. Always refer to the specific reference range printed on your lab report.)
Interpreting Your CBC Test Results
When you receive your CBC test results, the platelet count is not the only number you should analyze. Modern hematology analyzers provide indices that give context to the count.
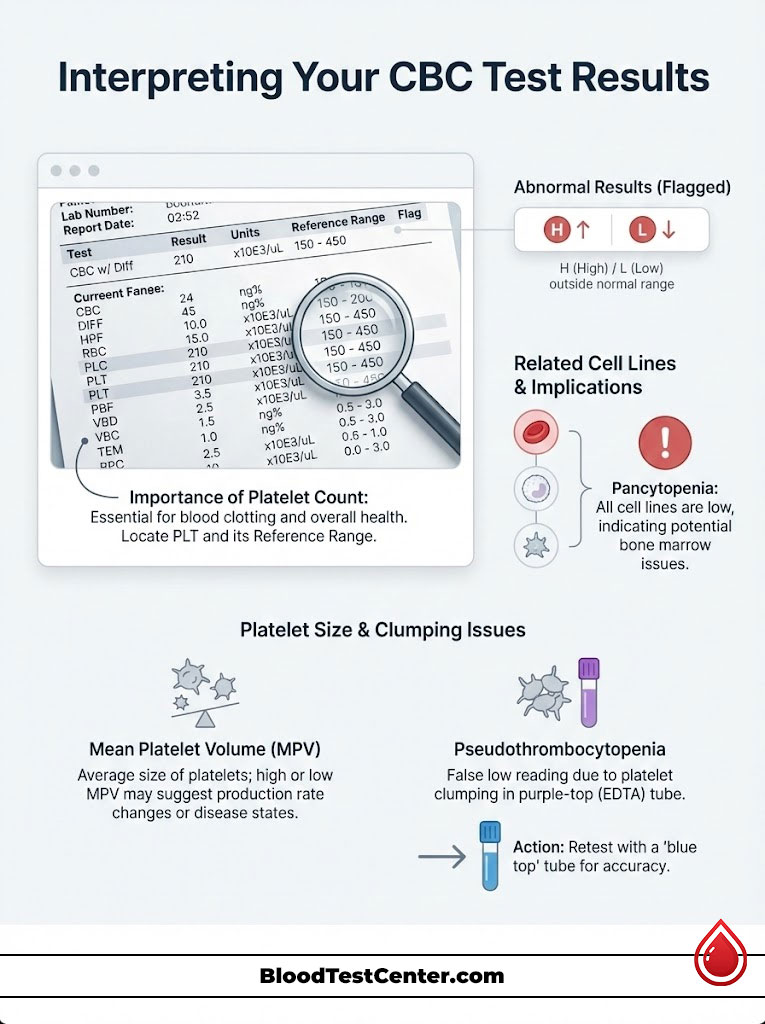
How to Read the Numbers
Look for the abbreviation “PLT” on your lab report. Next to your result, there will be a column labeled “Reference Range.” If your number is outside this column, it will likely be flagged with an “H” (High) or “L” (Low).
It is crucial to look at the other cell lines. If your red blood cells and white blood cells are also abnormal, it points to a “pancytopenia” (all cells low), which suggests a more systemic bone marrow issue. If only the platelets are off, the list of potential causes narrows significantly.
Mean Platelet Volume (MPV) Explained
One of the most valuable secondary keywords on your report is Mean Platelet Volume (MPV). This measures the average physical size of your platelets.
Young, newly produced platelets are large and robust. As they age in circulation, they get smaller. Therefore, the MPV tells the doctor how hard the bone marrow is working.
- High MPV with Low Platelet Count: This is actually a “good” sign in a bad situation. It means your body is destroying platelets (perhaps due to an autoimmune issue like ITP), but the bone marrow is responding vigorously by pumping out massive, young platelets to compensate.
- Low MPV with Low Platelet Count: This is more concerning. It suggests the bone marrow is “under-producing” or failing to make new cells, which occurs in conditions like aplastic anemia or during chemotherapy.
Pseudothrombocytopenia (False Lows)
Before accepting a diagnosis of thrombocytopenia, doctors must rule out a lab error known as pseudothrombocytopenia. This happens when the anticoagulant in the test tube (EDTA) causes your platelets to clump together. The machine misreads these large clumps as white blood cells or ignores them, reporting a falsely low platelet count.
If you have no symptoms of bleeding but a very low count, your doctor may request a re-test using a “blue top” tube (citrate) to get an accurate number.
Thrombocytopenia: When Counts are Too Low
A low platelet count (thrombocytopenia) is the most common platelet disorder encountered in hospitals. The urgency of treatment depends entirely on the severity of the deficit.
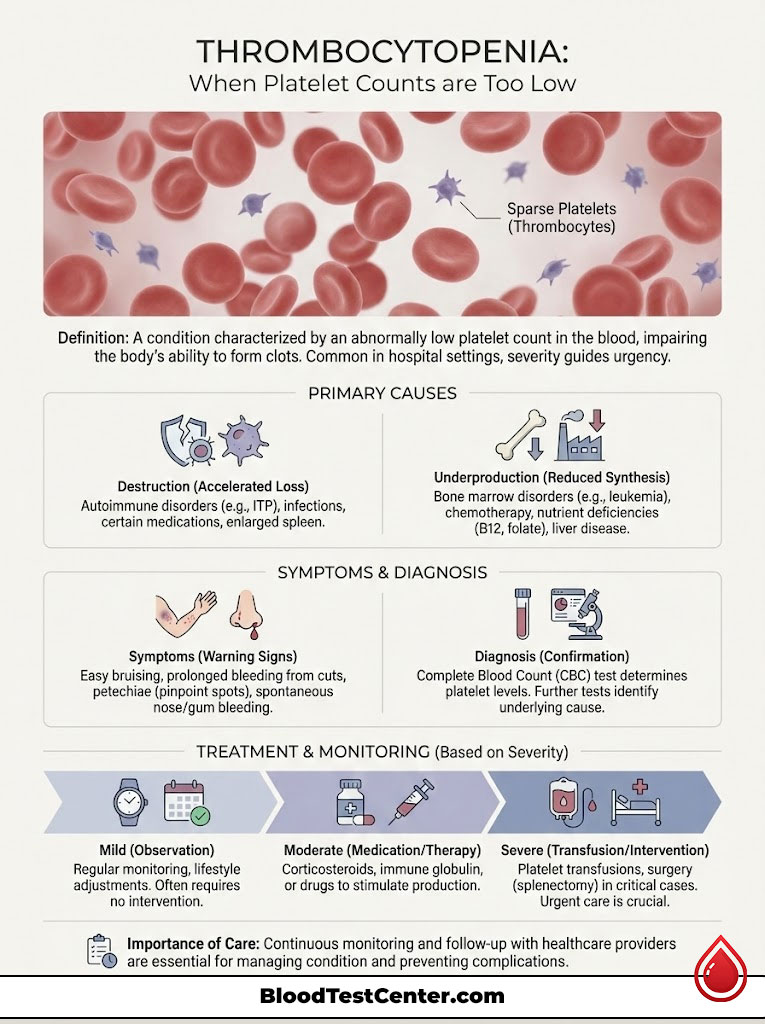
Defining the Severity Levels
- Mild (100,000 – 149,000/mcL): This is very common. It is rarely treated. Doctors usually adopt a “watch and wait” approach to see if it resolves or stabilizes.
- Moderate (50,000 – 99,000/mcL): This level requires investigation. While you are unlikely to bleed spontaneously, you are at risk if you get into a car accident or need surgery.
- Severe (Below 20,000 – 50,000/mcL): This is the danger zone.
- Critical (Below 10,000 – 20,000/mcL): At this level, spontaneous intracranial hemorrhage (bleeding in the brain) or internal GI bleeding becomes a real risk. Hospitalization is often required.
Common Causes of Low Platelets
The causes of low platelet count are vast, but they generally fall into two buckets: destruction or underproduction.
- Viral Infections: Viruses are notorious for temporarily suppressing bone marrow. HIV, Hepatitis C, Epstein-Barr (Mononucleosis), and Dengue fever are common culprits.
- Nutrient Deficiencies: Your marrow requires specific fuel to create cells. A severe lack of Vitamin B12 or Folate can halt platelet production.
- Autoimmune Conditions: In Idiopathic Thrombocytopenic Purpura (ITP), the body’s immune system mistakenly attacks its own platelets. Lupus and Rheumatoid Arthritis can also trigger this destruction.
- Medications: Certain drugs, including heparin (a blood thinner), antibiotics (sulfa drugs), and chemotherapy agents, can decimate platelet levels.
- Alcohol Toxicity: Heavy alcohol consumption is directly toxic to the bone marrow and often leads to low platelet counts combined with liver issues.
Symptoms of Low Platelets
The body gives clear warning signs when hemostasis is failing.
- Petechiae: These are tiny, pinpoint red or purple dots that usually appear on the lower legs. They result from microscopic capillaries leaking blood under the skin.
- Purpura: These are larger, unexplained bruises that appear without trauma.
- Mucosal Bleeding: You may notice blood on your toothbrush after gentle brushing, frequent nosebleeds that are hard to stop, or exceptionally heavy menstrual periods.
Thrombocytosis: When Counts are Too High
On the other side of the spectrum is thrombocytosis, or a high platelet count. This condition is often discovered accidentally during a routine physical, as it is frequently asymptomatic in its early stages.
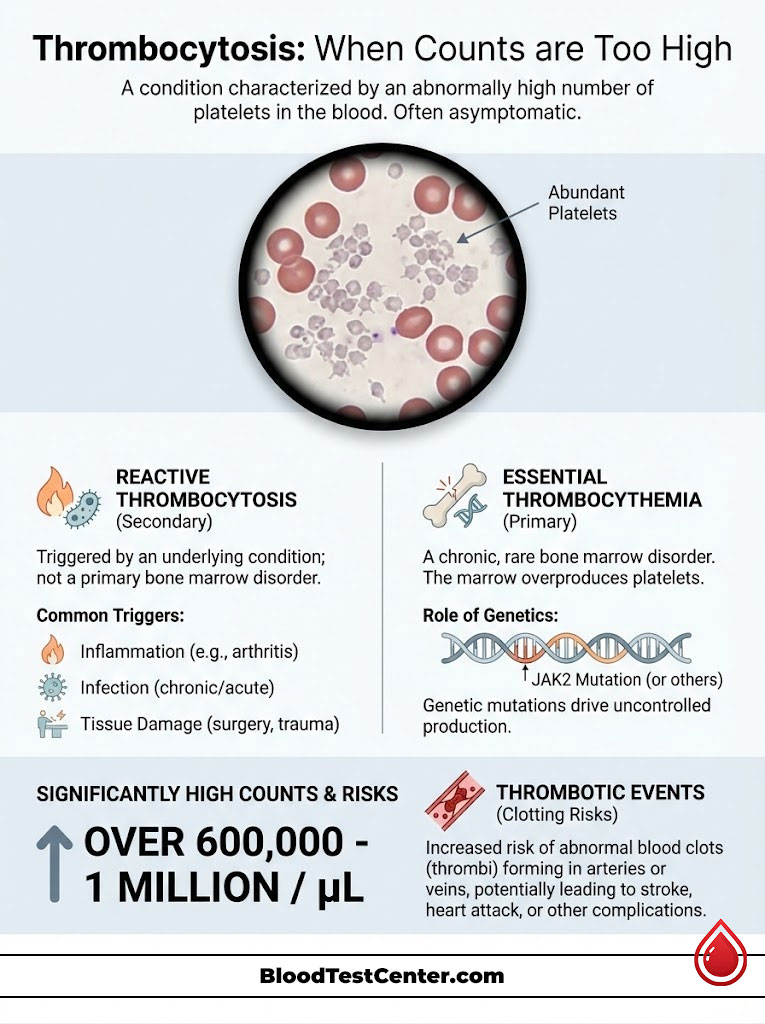
Reactive Thrombocytosis (Secondary)
This accounts for the majority of high platelet cases. “Reactive” means the high count is a reaction to something else happening in the body. When you have inflammation, infection, or tissue damage, the body releases cytokines that stimulate platelet production.
Common triggers include:
- Recent surgery or trauma (the body ramps up clotting ability to heal wounds).
- Iron deficiency anemia: Paradoxically, low iron can signal the marrow to overproduce platelets.
- Removal of the spleen (Splenectomy): Without the spleen to store platelets, they all circulate in the bloodstream, leading to permanently higher counts.
Essential Thrombocythemia (Primary)
This is a chronic condition where the bone marrow itself is faulty. It is a type of Myeloproliferative Neoplasm (MPN). In Essential Thrombocythemia, the megakaryocytes are hyperactive, often due to a genetic mutation such as JAK2.
Patients with this condition have persistently high platelet counts (often over 600,000 or even 1 million) without any external infection or cause.
Risks of High Platelets
The danger of high platelet count is twofold.
- Clotting (Thrombosis): The blood becomes “sticky.” This increases the risk of Deep Vein Thrombosis (DVT), Pulmonary Embolism, Heart Attack, or Stroke.
- Paradoxical Bleeding: It sounds contradictory, but when counts get extremely high (over 1 million), the platelets can use up a specific protein called Von Willebrand factor. This leads to a type of acquired bleeding disorder where the blood cannot clot despite the high number of platelets.
Comparison of Abnormal States
To help clarify the differences between these two extremes, the table below outlines the key distinctions between thrombocytopenia and thrombocytosis.
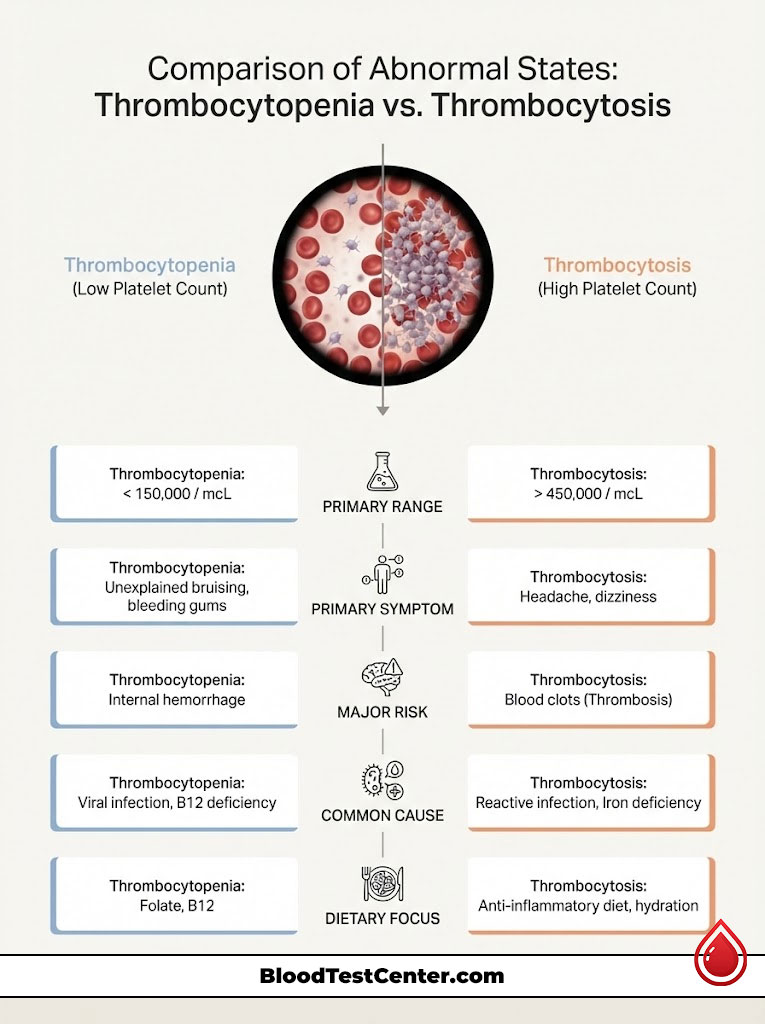
| Feature | Thrombocytopenia (Low) | Thrombocytosis (High) |
| Primary Range | < 150,000 / mcL | > 450,000 / mcL |
| Primary Symptom | Unexplained bruising, petechiae, bleeding gums. | Headache, dizziness, visual changes, burning hands/feet. |
| Major Risk | Internal hemorrhage (Brain/Gut). | Blood clots (Stroke/DVT/Heart Attack). |
| Common Cause | Viral infection, ITP, Alcohol, B12 deficiency. | Infection (Reactive), Essential Thrombocythemia, Iron deficiency. |
| Dietary Focus | Folate, B12, Iron-rich foods. | Anti-inflammatory diet, hydration to prevent viscosity. |
When to See a Doctor: Surgical and Emergency Thresholds
Knowing your number is one thing; knowing when to act is another. Medical professionals use specific thresholds to determine safety for procedures.
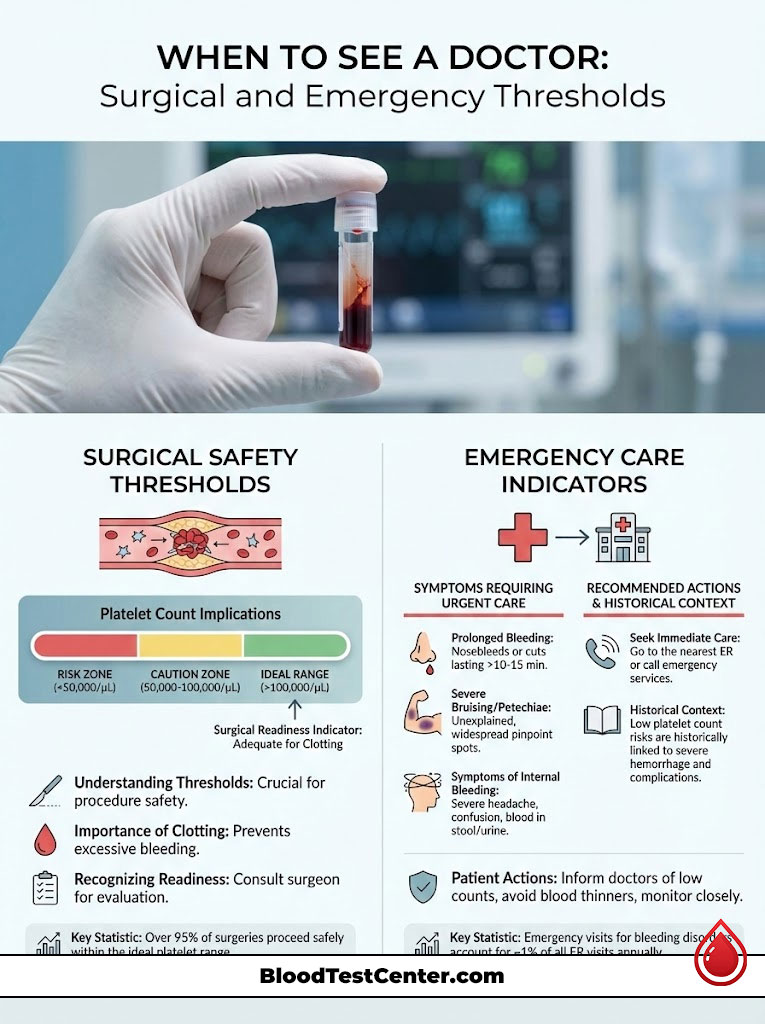
The “Safe” Numbers for Surgery
Surgeons are risk-averse. They need to ensure that if they make an incision, the blood will clot.
- Neurosurgery and Eye Surgery: These are high-risk areas. Surgeons typically require a platelet count above 100,000/mcL.
- General Surgery and Epidurals: For most abdominal surgeries or childbirth epidurals, a count above 50,000 to 80,000/mcL is considered safe.
- Dentistry: Routine extractions and cleanings can usually proceed safely with a count above 50,000/mcL.
When to Go to the ER
If you have a known history of low platelet count, you must be vigilant. You should seek emergency care if:
- Your count drops below 20,000/mcL.
- You experience a nosebleed that does not stop after 10 minutes of pressure.
- You see blood in your stool (which may appear black/tarry) or vomit that looks like coffee grounds.
- You develop a sudden, severe headache (potential brain bleed).
Lifestyle Factors and Management
While many platelet disorders require medical intervention, lifestyle plays a supportive role in maintaining a normal platelet count.
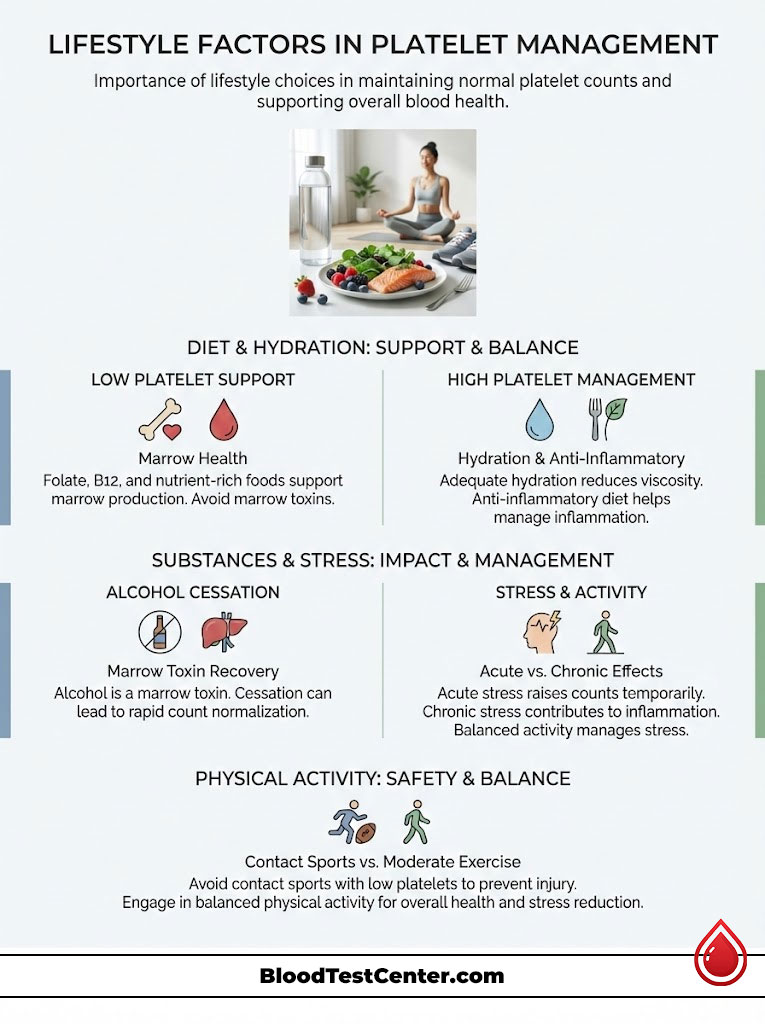
Diet and Nutrition
For those with low platelets, nutrition is about providing the building blocks for the marrow.
- Folate: Found in dark leafy greens, beans, and peanuts.
- Vitamin B12: Found in eggs, meat, and fortified cereals.
- Papaya Leaf Extract: Several studies have suggested that papaya leaf extract may help boost platelet production, particularly in cases of Dengue fever, though it should not replace medical treatment.
For those with high platelets, hydration is key to preventing the blood from becoming too viscous (thick). An anti-inflammatory diet rich in Omega-3 fatty acids may help reduce the “stickiness” of platelets, though it will not lower the count itself.
Alcohol and Toxins
Alcohol is a marrow toxin. For someone with borderline low platelet count, quitting alcohol is the single most effective lifestyle change. It removes the suppressive toxin and allows the marrow to regenerate. Often, drinkers with counts in the 80,000 range see a return to normal platelet count ranges within weeks of cessation.
Stress and Physical Activity
Can stress cause abnormal platelet levels? Acute physiological stress (like a car accident) causes the spleen to dump platelets into the bloodstream, raising the count temporarily. Chronic stress may contribute to inflammation, which can keep counts reactive.
If you have low platelets (below 50,000), doctors will advise against contact sports like football or wrestling. A minor impact that causes a bruise in a healthy person could cause a massive internal hematoma in someone with thrombocytopenia.
Summary & Key Takeaways
Your platelet count is a vital window into your hematological health. A normal platelet count range of 150,000 to 450,000 ensures your body can handle day-to-day repairs without risk of clotting or bleeding.
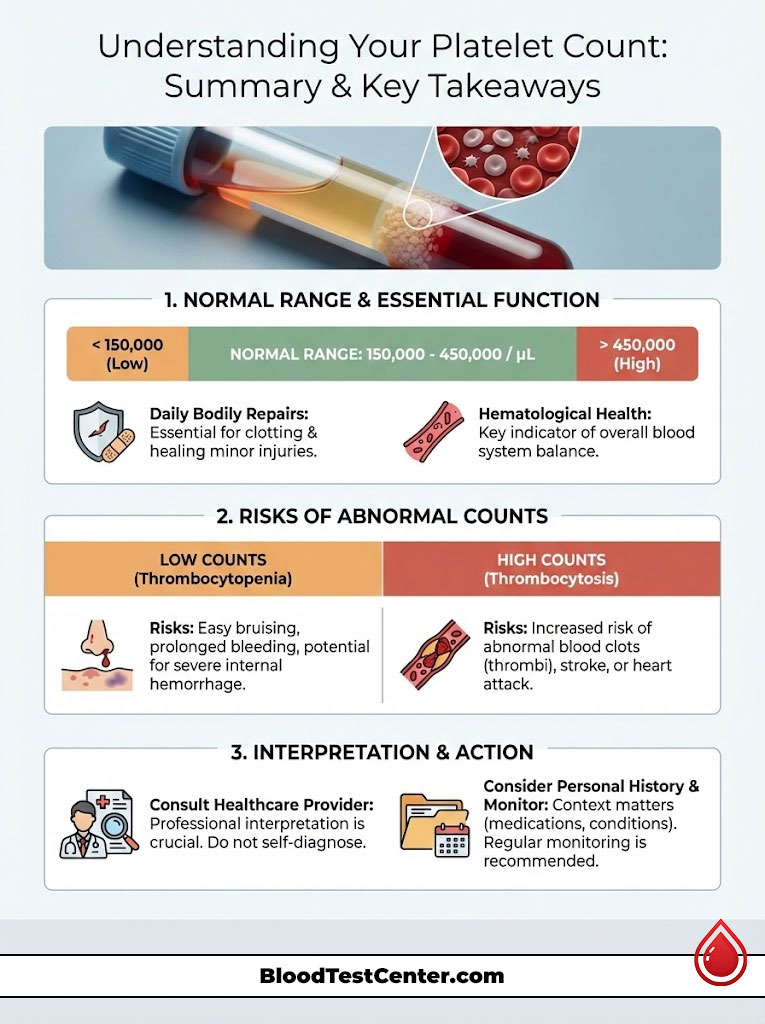
- Low Platelet Count (Thrombocytopenia): Usually caused by viral infections, nutrient deficiencies, or immune disorders. Watch for bruising and petechiae.
- High Platelet Count (Thrombocytosis): Often a reaction to inflammation or iron deficiency. Watch for headaches and clotting risks.
- Context Matters: A number slightly outside the range is rarely an emergency. Trends over time, MPV results, and physical symptoms provide the full picture.
Always interpret your CBC test results in consultation with a healthcare provider who understands your full medical history.
Frequently Asked Questions (FAQs)
Is a platelet count of 145,000 considered dangerous?
No, a count of 145,000 is only marginally below the standard threshold. It is considered mild thrombocytopenia and is generally benign. Most doctors will simply monitor this level during annual check-ups unless you have active bleeding symptoms.
What cancers cause high platelet counts?
While infection is the most common cause, certain blood cancers like Essential Thrombocythemia (ET), Chronic Myeloid Leukemia (CML), and Polycythemia Vera can cause persistently high counts. Some solid tumors (lung, colon) can also cause reactive high platelets due to inflammation.
Can dehydration cause high platelets?
Yes. When you are severely dehydrated, the volume of plasma (liquid) in your blood decreases. This makes the blood more concentrated, causing a condition called hemoconcentration, which can falsely elevate the platelet count on a lab test.
How fast can platelet counts drop?
In acute conditions like sepsis or acute ITP, platelet counts can drop precipitously within 24 to 48 hours. This is why frequent blood draws are necessary for hospitalized patients with unstable counts.
What happens if platelets are too low during surgery?
If platelets are too low, the blood cannot form a clot to close the surgical incision. This leads to uncontrolled oozing, hematomas, and potentially life-threatening blood loss. Surgeons may order a platelet transfusion before operating if the count is critical.
Does Vitamin D affect platelet count?
Current research is mixed, but Vitamin D plays a role in regulating the immune system. Since many low platelet conditions are autoimmune (like ITP), correcting a Vitamin D deficiency may support overall immune health, though it is not a direct cure for low platelets.
Why do heavy drinkers often have low platelets?
Alcohol has a double-negative effect: it directly suppresses platelet production in the bone marrow and often causes liver damage (cirrhosis), which leads to an enlarged spleen that traps the platelets that are produced.
Can I fly on an airplane with low platelets?
If your count is stable and above 40,000 or 50,000, flying is generally safe. However, if counts are very low, the changes in cabin pressure and the risk of trauma from turbulence may be a concern. Always consult your hematologist before travel.
What is the life expectancy with Essential Thrombocythemia?
With proper management (aspirin, medication to lower counts), people with Essential Thrombocythemia often have a near-normal life expectancy. The main goal is preventing clots and strokes.
Do antibiotics lower platelet count?
Yes, certain antibiotics can trigger drug-induced thrombocytopenia. Sulfa drugs, penicillin, and vancomycin are known to occasionally cause the immune system to attack platelets.
Is 450,000 platelets high for a woman?
It is at the very upper limit of normal. Since women often have higher baseline counts than men, 450,000 might be “normal” for your specific physiology, but it warrants monitoring to ensure it does not continue to rise.
How do I raise my platelet count naturally?
While you cannot force the marrow to produce cells if there is a medical blockage, you can support it by eating foods rich in Folate (leafy greens), Vitamin B12, and Iron. Avoiding alcohol and quinine (found in tonic water) also prevents unnecessary platelet destruction.
Disclaimer: The content provided in this article is for educational and informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or blood test result. Never disregard professional medical advice or delay in seeking it because of something you have read online.
References:
- National Heart, Lung, and Blood Institute (NHLBI). “Thrombocytopenia (Low Platelet Count).”
- Mayo Clinic. “Thrombocytosis (High Platelet Count).”
- American Society of Hematology. “Blood Basics: Platelets.”
- Cleveland Clinic. “Mean Platelet Volume (MPV) Test.”